To read or download this Journal in a magazine format on ISSUU, please click here
AIMS Journal, 2019, Vol 31, No 1
By Katie Hickey
One of the most well-known medical sayings is, “First, do not harm”. This phrase appears in the Hippocratic Corpus, specifically in Epidemics, book I, sect. XI: 'The physician must... have two special objects in view with regard to disease, namely, to do good or to do no harm'. 1
In our current developed society we are extremely fortunate to have advanced medicine at our fingertips. Countless lives are now saved thanks to modern medicine, access to antibiotics, sterile surgical techniques and general improvements in nutrition. With around a quarter of all births in the UK ending in caesarean section and over a third of all labours artificially induced, one might be forgiven for thinking women in our modern society have lost the ability to give birth without medical intervention. In 1860 Oliver Wendell Holmes Senior famously remarked in a lecture to the Massachusetts Medical Society, “If the whole materia medica, as now used, could be sunk to the bottom of the sea, it would be all the better for mankind—and all the worse for the fishes.’ He observed that the injuries caused by overmedication were often masked by the disease1. 160 years later we are still striving to find the right balance and the appropriate use of medicine, particularly in the context of maternity services.
The proportion of births where labour was induced has increased from 20.4 per cent in 2007-08 to 32.6 per cent in 2017-182. Many women and birth professionals are left asking why? How can the rates of induction be rising so sharply? How much harm are we causing to women and their babies with these high rates of intervention? Are any outcomes improved?
In order to understand why the rates of induction are soaring, and how this is impacting women, we need to try to understand the current climate and culture of our maternity system. This sets the scene for the rest of our conversations on the issue. It is also important to put ourselves in the position of health care providers and to understand what pressures they are under. This surely helps us to navigate the current maternity system and often helps to provide much needed context to these emotive and important conversations.
Stillbirth in the UK
Historically, the stillbirth rate in the UK has lagged behind other high- income countries; in 2015, the UK ranked 24th out of 49 high income countries and the annual rate of reduction of 1.4% is significantly lower than comparable countries (e.g. 6.8% in the Netherlands) with about a 33% variation in rates between regions.3 In 2016, a series of articles in the Lancet called for efforts to address the disparity in stillbirth rates between, as well as within, individual countries.4 Reducing the numbers of deaths of babies before birth remains a challenge to maternity services in high-income countries. In the UK, the majority of stillbirths occur in the antenatal period (~90%) and occur in normally-formed babies.3
The 2015 MBRRACE-UK enquiry found that there was a collection of failures in the care women received that contributed to the continued high rate of stillbirth in the UK. Their findings also sadly showed the same care issues being repeated since their previous enquiry 15 years earlier.5
There is a huge drive to reduce the national stillbirth rate in the UK, and of course this is a very welcome endeavour. In November 2015, the Secretary of State for Health announced a national ambition to halve the rates of stillbirths, neonatal and maternal deaths and intrapartum brain injuries by 2030, with a 20% reduction by 20206. The NHS has produced a variety of new ‘care bundles’ and guidelines in an attempt to address the issue. Two of these care bundles are “Saving Babies Lives” and “Each Baby Counts”. I will look at both of these in more detail below.
At AIMS we are increasingly aware of the culture of fear in our maternity system and how this is used to disempower women, especially if they choose to give birth on their own terms. The fear of stillbirth is understandably one of the biggest fears of both parents and medical care givers and the new ‘care bundles’ discussed below have fed into the large increase in the induction rate in the UK.
What is a care bundle?
Care bundles are a small set of practices performed collectively and reliably with the intention of improving the quality of care. Some of these practices are based on evidence and some are not. Care bundles are used widely across healthcare settings with the aim of preventing and managing different health conditions.7 A 2017 systematic review designed to determine the effects of care bundles on patient outcomes and the behaviour of healthcare workers in relation to fidelity with care bundles, showed the effect of care bundles on patient outcomes is uncertain. 7
What happens when evidence is lacking?
In so many elements of maternity care, evidence-based medicine is not possible due to a complete lack of high quality evidence. There are many examples of maternity policies that are actually not based on evidence and many examples of common practice that go against best evidence (continuous electronic foetal monitoring for example8). This leaves medical professionals searching for what they would consider to be “best practice,” based on their best guess, in an attempt to bridge that gap where evidence is lacking. For women navigating the maternity system it’s really important to get an understanding of these differences, especially when it is not made clear by the medical staff what is based on evidence and what is their best guess.
Saving Babies’ Lives Care Bundle
The first version of the Saving Babies’ Lives Care Bundle (SBLCB) was published in March 2016 and it focussed predominantly on reducing the UK stillbirth rate. In November 2017, the ambition was extended to include reducing the rate of preterm births from 8% to 6% and the date to achieve the ambition was brought forward to 2025.6
A second version of this care bundle was published in March 2019. It brings together five elements of care that are recognised as evidence-based and/or best practice (noting that these two are very much not the same thing as discussed above).
The 5 elements of this care bundle are:
1. Reducing smoking in pregnancy
2. Risk assessment and surveillance for foetal growth restriction
3. Raising awareness of reduced foetal movement
4. Effective foetal monitoring during labour
5. Reducing preterm birth
Let’s look at these elements in some more detail and pick out where evidence either supports or contradicts the proposal in the care bundle:
1. Reducing smoking in pregnancy
This is based on strong, high quality evidence. Reducing smoking in pregnancy decreases the risk of stillbirth. A meta-analysis of seven studies showed that the risk of stillbirth was 52% higher in pregnant women who smoked 10 or more cigarettes per day than those who did not smoke. It was 9% higher for those smoking one to nine cigarettes a day.9
NICE’s Eyes on Evidence update, which provides commentary on important new evidence, said that a pooled analysis of 24 studies, which had more than eight million participants, found that the risk of stillbirth was 47% higher in women who smoked during pregnancy than in women who did not smoke while pregnant.
There is strong evidence that reducing smoking in pregnancy also impacts positively on many other smoking-related pregnancy complications, such as preterm birth, miscarriage, low birthweight and Sudden Infant Death Syndrome (SIDS). Whether or not a woman smokes during her pregnancy has a far-reaching impact on the health of the child throughout his or her life.6
A large proportion of women referred for smoking cessation report not attending their referral appointment. The provision and type of smoking cessation service offered to women is variable across the Trusts. In many areas smoking cessation services are not provided within maternity services and require referral to another location or care provider, these included referrals to external services, GPs and pharmacies. This need for additional referral may act as a practical barrier or a disincentive for women to attend these appointments. In addition, three Trusts did not offer referral due to withdrawal of funding for smoking cessation.10
This element of the SBLCB has the potential to reduce stillbirths significantly and it is supported by high quality evidence. If women cannot easily access smoking cessation services which are right for them, the opportunity for positive change is lacking.
2. Risk assessment and surveillance for foetal growth restriction
The identification of foetal growth restriction represents one of the main known clinical factors on the pathway to stillbirth.6 The measurement of foetal growth is far from an exact science. Fundal height measurement and ultrasound, as tools for estimating foetal size, have fairly large margins of error.
The 2015 MBRRACE-UK enquiry found that the main areas of concern for stillbirth were unchanged since the previous enquiry 15 years previously. This enquiry found missed opportunities when growth of the foetus was measured but not plotted on a growth chart and the identification of babies at risk of decreased growth was missed. Sadly even in cases where these babies were identified and plotted on said growth charts no action appeared to be taken, potentially leading to the loss of those babies lives.5
The results show that the detection in the number of babies that are small for gestational age (SGA), defined as an estimated fetal weight below the 10th centile at last ultrasound scan, has significantly increased during the implementation of the SBLCB. This can be seen as a positive step to reducing the national stillbirth rate.
In an attempt to capture all babies that are small for gestational age it has however led to an increase in the number of unnecessary inductions of labour for many women who may not have been at risk of stillbirth. There are serious risks associated with pre-term and early term inductions that are discussed below.
3. Raising awareness of reduced foetal movement
This element of the care bundle is focussed on raising awareness amongst pregnant women of the importance of reporting reduced foetal movements (RFM), and ensuring providers have protocols in place, based on best available evidence, to manage care for women who report RFM6. Findings from the 8th Report of the Confidential Enquiry into Stillbirths and Deaths in Infancy and the 2015 MBRRACE-UK Confidential Enquiry into Antepartum Stillbirth found that unrecognised or inappropriately managed episodes of RFM are contributory factors to avoidable stillbirths.
The AFFIRM study found that a care bundle which recommended all women have an ultrasound assessment of foetal wellbeing following presentation with RFM after 26 weeks’ gestation, and offered induction of labour for recurrent episodes of RFM after 37 weeks’ gestation did not significantly reduce stillbirths.
We do not fully understand how a decrease in movements is linked to stillbirth and even when we increase awareness and intervention the results show a disappointing impact to the rate of stillbirth.
The evaluation into implementation of the SBLCB10 showed 49% of women said they were concerned that their baby’s movements had slowed or stopped in their current pregnancy when explicitly asked. A high proportion of women perceiving RFM attended their maternity unit (77.3%). of those women attending their maternity unit with RFM, 74% received foetal heart monitoring, 65% of women received an ultrasound scan; 20% at every visit. Half were scanned within 24 hours and 20% of women were scanned within 2 to 3 days. 55% percent of women reporting RFM had induction of labour. You can see how this element of the care bundle has contributed significantly to the increases in the national induction rate.
One of the key interventions in elements 2 and 3 of the SBLCB, discussed above, is offering early birth for women at perceived risk of stillbirth. The Avoiding Term Admissions Into Neonatal units (Atain) programme has identified that babies born at 37 – 38 weeks gestation were twice as likely to be admitted to a neonatal unit than babies born at later gestations. There are also concerns about long term outcomes following early term birth (defined as 37 and 38 weeks). These concerns relate to potential long term adverse effects on the baby due to birth prior to reaching maturity, for example, the baby’s brain continues to develop in-utero at term. One example is the risk that the child will subsequently have a special educational needs (SEN). The risk of this outcome is about 50% among infants born at 24 weeks of gestational age and it progressively falls with increasing gestational age at birth, only to bottom out at around 40 – 41 weeks6.
Health care providers must be cautious about recommending induction of labour for perceived reduction of foetal movements in the absence of evidence of compromise to the baby. That being said poorly managed episodes of RFM have been highlighted in previous enquiries into stillbirth as missed opportunities to reduce the stillbirth rate. There is no easy answer as yet.
4. Effective foetal monitoring during labour
In 2017 a Cochrane review asked the question: “Is continuous cardiotocography (CTG) to electronically monitor babies' heartbeats and wellbeing during labour better at identifying problems than listening intermittently?” The findings were that CTG during labour is associated with reduced rates of neonatal seizures, but no clear differences in cerebral palsy, infant mortality or other standard measures of neonatal wellbeing. However, continuous CTG was associated with an increase in caesarean sections and instrumental vaginal births compared to intermittent monitoring.
The use of foetal heart rate monitoring of any kind is not based on evidence. We do not know if monitoring foetal heart rates, even intermittently, improves outcomes for mothers and babies. It is based on an assumption that it will improve outcomes but it is that same assumption that leads to continuous CTG being used more and more widely. Very interestingly, new NICE guidelines on caring for women having a vaginal birth after a previous caesarean (VBAC) now clearly state that there is no evidence to support routine use of continuous CTG for these births, despite it being defined as a “high risk” birth in the eyes of the medical care givers 11.
Continuous CTG monitoring is still used as standard on labour wards across the country without evidence that it improves outcomes, and with evidence that it causes harm. We do know it can massively impact a woman’s ability to cope with labour as it restricts mobility and often leads to further interventions such as epidural and caesarean birth.
The INFANT Trial was set up to find out whether computer software (produced by INFANT K2 Medical Systems) which provided interpretation of continuous electronic foetal monitoring (EFM) to support decisions about care in labour for women having continuous EFM could reduce birth injury and stillbirth compared with continuous EFM used on its own. You can read AIMS’ summary of the research here: www.aims.org.uk/journal/item/infant-trial
The INFANT Trial team’s conclusion was that ‘…use of computerised interpretation of cardiotocographs in women who have continuous electronic foetal monitoring in labour does not improve clinical outcomes for mothers or babies.’
5- Reducing preterm birth
Preterm birth (PTB), defined as birth at less than 37+0 week’s gestation, is a common complication of pregnancy, comprising around 8% of births in England and Wales12. Babies born preterm have high rates of early, late, and post-neonatal mortality and morbidity.
We know from MBRRACE-UK surveillance data that 70% of all stillbirths and neonatal deaths occur in babies born before term and nearly 40% are extremely preterm, being born before 28 weeks’ gestation.
This element of the care bundle is new and is seen as an addition to the second version of the SBCLB. It aims to better predict those babies who are at risk of preterm birth and treat, where possible, to try and prevent preterm birth. For those babies where preterm birth is unavoidable then appropriate care in specialist facilities should be arranged (many babies are currently born in facilities that are unable to cope with their medical needs appropriately). Analysis of data from the National Neonatal Research Database has shown that extremely preterm birth outside an obstetric unit co-located with a tertiary neonatal intensive care unit (NICU) is associated with a 50% increase in neonatal death or severe brain injury, yet in 2016 approximately 1 in 3 extremely preterm births were in a hospital without a NICU6.
It has been acknowledged that the NHS will not achieve the national Maternity Safety Ambition to halve the rates of stillbirths, neonatal and brain injuries that occur during or soon after birth by 2030, unless the rate of preterm births is reduced. The Government then set an additional ambition to reduce the national rate of preterm births from 8% to 6%. It is hoped that this new element of the SBLCB will contribute to the reduction of preterm birth.6
What has been shown so far.
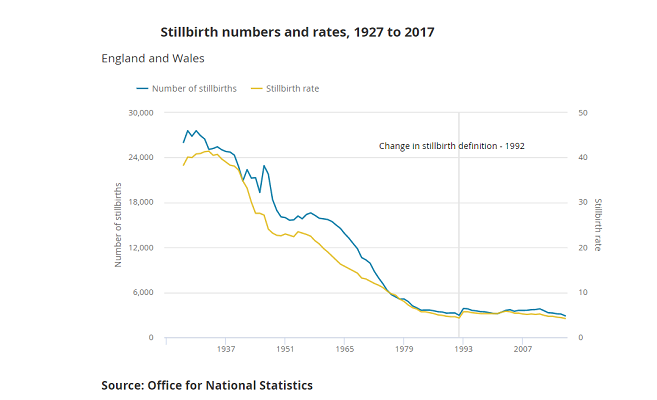
The UK stillbirth rate decreased to 4.2 per 1,000 total births in 2017, the lowest rate on record with figures available back to 1927; in the last decade since 2007 the stillbirth rate has decreased by 19.2% (ONS). In July 2018 a published evaluation of the implementation of the Saving Babies’ Lives Care Bundle in early adopter NHS Trusts in England10 showed the following results:
In participating Trusts, stillbirth rates have declined by 20% over the period during which the Saving Babies’ Lives Care Bundle (SBLCB) was implemented, although this improvement cannot be unambiguously attributed to the Care Bundle. The crude stillbirth rate was 4.14/1,000 births before SBLCB and 3.31/1,000 births after SBLCB. Term singleton stillbirths declined by 22% over the same period. There was no demonstrable relationship between stillbirth rates and the overall implementation score for the SBLCB.
Significant variation in the stillbirth rate persists across the early adopter Trusts beyond that explicable by care level and aggregated deprivation score. This suggests that there may be variation in practice between Trusts and therefore scope for improvement in some. Associations with deprivation suggest a need for wider scale social and public health policy changes to tackle inequality in addition to the SBLCB if the stillbirth rate is to be further reduced.
It was not possible to determine whether implementation of SBLCB or any of its individual components per se reduces stillbirth or affects any of the associated clinical and service outcomes. However, due to the nature of the interventions it is highly plausible that SBLCB contributed to the continued improvement in stillbirth rate in the early adopter Trusts.
There has been a large impact to maternity services and a knock-on effect to women and their babies:
Following implementation of the SBLCB in study sites, the number of ultrasound scans performed increased (by 25.7%) as did interventions at or around the time of birth including induction of labour (by 19.4%) and emergency caesarean section (by 9.5%). The number of elective caesarean sections also increased over the timeframe of this analysis (by 19.5%)
Rates of preterm birth, admission to a neonatal unit and the number of babies receiving therapeutic cooling have increased in study sites during the timeframe of the SBLCB evaluation; by 6.5%, 17.1% and 27.7% respectively.
Awareness of the SBLCB by staff was modest, with 42% of staff claiming to be unaware of it although staff were implementing all or part of the bundle as part of their daily practice. Awareness was lowest among frontline staff and highest in managers.
The methodological quality of clinical practice guidelines in relation to the SBLCB were generally of low quality and highly variable between Trusts.
Version 2 of SBLCB includes some excellent improvements on the first version. There is acknowledgement that during implementation of some of the elements of the care bundle there was an increase in interventions to women not really at risk. “It is recognised that the previous bundle imposed significant burdens on service providers. In particular, increased numbers of ultrasound scans and increased rates of induction of labour and emergency caesarean sections were observed. By being more specific this bundle (version 2) will help focus intervention more in pregnancies genuinely at risk of complication.....there are opportunities to reduce obstetric intervention.”
This second version really urges care providers to think more carefully and to avoid intervention unless there is clear evidence of compromise to the baby. It also reminds them to "be vigilant to include women in the decision-making process" which is a very unfortunate turn of phrase as it implies that women are only to be "included" in the decision making - whereas in fact the decisions about what to accept or decline can only be made by the woman. This was something that was distinctly lacking in the first version of this care bundle and the changes are very welcomed. SBLCB version 2.... “highlights the important principles of good communication, choice and personalisation which help empower women to be involved in decision making about their care. A good way to apply these principles is through the implementation of continuity of carer...” What a relief to see this point acknowledged, but we shall wait to see how this trickles down to front line staff who need to understand the importance of these aspects of the care they provide. It’s sad that these elements were missing from the first version of the bundle.
Each Baby Counts
Each Baby Counts has the aim to halve the UK’s national rate of stillbirth, maternal and neonatal deaths and brain injuries that occur during, or soon after birth, by 2025. It is aiming to do this by investigating every stillbirth case reported to them and identifying avoidable factors in every case. The programme also recognises the impact that each of these tragic events has on parents and families. The aim is to ensure that maternity services learn from mistakes to reduce and prevent avoidable harm wherever possible.
The 2018 progress report for Each Baby Counts13 makes for a sad read. The number of incidents where different care might have led to a different outcome still remains high. 71% of the babies might have had a different outcome with different care.
The report suggests that the reasons for stillbirth, early neonatal death and brain injuries are complex and multifactorial. For the babies reported to Each Baby Counts, the reviewers concluded that there was rarely one single cause of the stillbirth, early neonatal death or brain injury. Rather, on average, there were 7 critical contributory factors leading to these devastating outcomes. This complexity and interdependency highlights the need for continued investment to improve care for women and babies across the UK. We are aware that this is not a case-controlled trial but an audit, so the results and conclusions need to be interpreted with caution – we don’t know how many of the babies who were fine would also have experienced some of these contributory factors.
Lack of consistent care
AIMS often hears from women who seem to be hounded incessantly, bordering on harassment by their health care providers. Some are coerced at every opportunity to agree to a particular intervention for, they say, the safety of their baby’s life when there is very often no evidence that a specific baby is at risk (see the AIMS article “beware the dead baby card14”). And yet, clearly other women are still falling through the gaps and are not being given the care and attention they need. With the current reports indicating nearly three quarters of babies who’ve died or been seriously injured during birth could have different outcomes with different care, this lack of attention to women is extremely worrying.
The maternity services are increasingly over-stretched. Low staffing levels, staff burn out, lack of training and support are key elements that prevent women receiving high quality care. A 2018 paper in the British Journal of Midwifery focussed on how women get information and make decisions regarding induction of labour and they found midwives presented induction as the preferred option, and alternative care plans, or the relative risks of induction versus continued pregnancy, were rarely discussed. Women reported that midwives often appeared rushed, with little time for discussion15. With 42% of health care providers claiming no knowledge of the SBLCB10 one might question what is the point of the NHS spending £94M per year10 on implementing the care bundle?
We are left wondering how much influence the service users consulted on during the formation of these care bundles really has? Why has it taken until the second version of the SBLCB to place any attention on the way we deliver maternity services and the emphasis on women making decisions about their own bodies, babies and births? After all, it is women, and their babies, who are subjected to the consequences of practices, policies and guidelines.
Continuity of Carer
As well as focussing on medical intervention and technology we welcome the included focus on Continuity of Carer. When a woman is cared for by the same midwife throughout her pregnancy, birth and postnatal period outcomes improve dramatically. The relationship a woman forms with her midwife can literally make the difference between life and death.
The second version of SBLCB6 does highlight evidence that continuity models improve safety and outcomes. Women who receive Continuity of Carer are 16% less likely to lose their baby, 19% less likely to lose their baby before 24 weeks and 24% less likely to experience preterm birth. It says, this model of care will also be targeted towards women from BAME groups and those living in deprived areas, for whom midwifery-led continuity of carer is linked to significant improvements in clinical outcomes.6
Whilst this is a very welcomed addition to the care bundle we have to question why this isn’t a stand-alone element of the care bundle. Given that the evidence of benefit of Continuity of Carer is not new it is increasingly frustrating to not see this focussed on more specifically. It seems as though rolling out Continuity of Carer falls below the priority of using technology, machines and obstetric intervention time and time again and that is extremely disappointing.
The Albany Midwifery Practice is a shining example of how Continuity of Carer can provide outstanding outcomes for women16. The Albany Practice mostly cared for women from BAME origin in an area of high social deprivation in South East London. Despite these women being at higher risk for poor outcomes and increased intervention the results show the opposite. www.aims.org.uk/journal/item/the-albany-analysis . How many times do these lessons need to be relearnt before we see a significant change in the way maternity services are offered to women? Despite version 2 of the SBLCB highlighting how Continuity of Carer should be offered to women particularly from BAME backgrounds6, it remains to be seen if this is followed through.
When we have clear, unequivocal evidence that continuity of carer improves outcomes for women and babies16 why is the NHS not focussing more of its efforts on that? AIMS would like to see relationships (based on evidence of improving outcomes) replacing technology (not based on evidence of improving outcomes) wherever possible.
Conclusions
When we question why the rate of induction is rocketing in the UK it helps to have some understanding of the climate and culture of the maternity system today. “Your baby is better out than in” seems to be a common thought amongst health care providers and given the care bundles and guidelines which are in place it is hardly surprising that they feel this way.
We cannot turn a blind eye to the fact that induction of labour itself is not a benign procedure and has its own associated risks, some of which are the exact risks we are trying to avoid, hypoxic injury to newborns being one17. The 2018 report on the SBLCB showed rates of preterm birth, admission to a neonatal unit and the number of babies receiving therapeutic cooling have increased by 6.5%, 17.1% and 27.7% respectively (comparing rates before and after the implementation of the SBLCB). We cannot say at this time what effect these increasing interventions are going to be causing in the long term. However, with respect to mental and physical health of mothers and children, a 27.7% increase in therapeutic cooling (which is carried out for babies that have suffered hypoxic injury during birth) shows that many babies are indeed being damaged by the increase in induction of labour.
In an attempt to capture all babies at risk it has led to an increase in pre-term and early term inductions and caesarean sections. How can we look at this in terms of balancing harm vs good? The dilemma is that early term birth may reduce the risk of an uncommon but serious adverse event (stillbirth or neonatal death) while at the same time increases the risk of much more common adverse events which can also have devastating outcomes. Decision-making balances the risks of causing one form of harm to relatively large numbers of mothers and infants in order to prevent another form of harm to a relatively small number. For example, at 37 weeks, 10 inductions will lead to one additional baby being admitted for neonatal care but it will require more than 700 inductions to prevent each perinatal death.6
Does increasing the rate of induction of labour reduce the incidence of stillbirth? There is conflicting evidence and opinion. As there are so many changes happening in our maternity system at one time it is difficult to prove that one element out of many is the reason for a decrease in our national stillbirth rate. In an area so highly complex and emotive, coupled with uncertainty and the lack of unequivocal, unbiased scientific evidence, it is understandable that the rates of intervention have rocketed.
In the course of writing this article I have battled myself with how I feel about all of these elements and I am also eight months pregnant at the time of writing this piece. The death of a baby has lifelong consequences for the family who have suffered this tragedy. Induction of labour is not the only answer to reducing the stillbirth rate and, as we have discussed, it is not without its own risks that sometimes result in devastating outcomes.
Women MUST be at the centre of their care and decision making. Striking the balance between the use and overuse of medicine is not always easy, especially when the potential consequences either way are totally devastating. Only when women are given the time, respect and support that they deserve can we really see this balance being reached. Whilst women are not enabled to make truly informed decisions about their care, the offer of induction will continue to be problematic.
REFERENCES
1- BMJ 2013;347:f6426 First do no harm.
2- digital.nhs.uk/data-and-information/publications/statistical/nhs-maternity-statistics/2017-18
3- www.npeu.ox.ac.uk/downloads/files/mbrrace-uk/reports/MBRRACE-UK-PMS-Report-2014.pdf MBRRACE-UK Perinatal Mortality Surveillance Report, UK Perinatal Deaths from January to December 2014.
4- Flenady V, Wojcieszek AM, Middleton P, et al. Stillbirths: recall to action in high-income countries. Lancet. Feb 13 2016;387(10019):691-702.
5- www.hqip.org.uk/wp-content/uploads/2018/02/perinatal-confidential-enquiry-term-singleton-normally-formed-antepartum-stillbirth-report-2015.pdf
6- www.england.nhs.uk/wp-content/uploads/2019/03/Saving-Babies-Lives-Care-Bundle-Version-Two-Final-Version2.pdf
7- The effects of care bundles on patient outcomes: a systematic review and meta-analysis Implementation Science201712:142
implementationscience.biomedcentral.com/articles/10.1186/s13012-017-0670-0
8- www.cochrane.org/CD006066/PREG_continuous-cardiotocography-ctg-form-electronic-foetal-monitoring-efm-foetal-assessment-during-labour
9- Maternal smoking and the risk of still birth: systematic review and meta-analysis www.ncbi.nlm.nih.gov/pmc/articles/PMC4372174/
10- Evaluation of the implementation of the Saving Babies’ Lives Care Bundle in early adopter NHS Trusts in England. July 2018
www.manchester.ac.uk/discover/news/download/573936/evaluationoftheimplementationofthesavingbabieslivescarebundleinearlyadopternhstrustsinenglandjuly2018-2.pdf
11- www.nice.org.uk/guidance/ng121/chapter/Recommendations?fbclid=IwAR3FEM8QoS6HlKNrajPKztDtbvcZiL7dlGYIAKrbYJYDiMjWAD3KRNN_fOY#previous-caesarean-section
12- National Institute for Health and Care Excellence (2015). Preterm Labour and birth (NICE Guideline 25). Available from: www.nice.org.uk/guidance/ng25
13- www.rcog.org.uk/en/guidelines-research-services/audit-quality-improvement/each-baby-counts/reports-updates/each-baby-counts-2018-progress-report/
14- www.aims.org.uk/journal/item/beware-the-dead-baby-card
15- Induction of labour: How do women get information and make decisions? Findings of a qualitative study Published Online:12 Jan 2018 https://doi.org/10.12968/bjom.2018.26.1.22
16- Midwifery continuity of carer in an area of high socio-economic disadvantage in London: A retrospective analysis of Albany Midwifery Practice outcomes using routine data (1997–2009) Homer, Caroline SE et al. Midwifery, Volume 48 , 1 – 10 www.midwiferyjournal.com/article/S0266-6138(17)30151-1/abstract
17- Induction of labor and cerebral palsy: a population-based study in Norway. www.ncbi.nlm.nih.gov/pubmed/21275920
18- NHS England (2016) National Maternity Review: Better Births Improving outcomes of maternity services in England
www.england.nhs.uk/wp-content/uploads/2016/02/national-maternity-review-report.pdf
The AIMS Journal spearheads discussions about change and development in the maternity services..
AIMS Journal articles on the website go back to 1960, offering an important historical record of maternity issues over the past 60 years. Please check the date of the article because the situation that it discusses may have changed since it was published. We are also very aware that the language used in many articles may not be the language that AIMS would use today.
To contact the editors, please email: journal@aims.org.uk
We make the AIMS Journal freely available so that as many people as possible can benefit from the articles. If you found this article interesting please consider supporting us by becoming an AIMS member or making a donation. We are a small charity that accepts no commercial sponsorship, in order to preserve our reputation for providing impartial, evidence-based information.
AIMS supports all maternity service users to navigate the system as it exists, and campaigns for a system which truly meets the needs of all.