To read or download this Journal in a magazine format on ISSUU, please click here
AIMS Journal, 2018, Vol 30, No 3
By Debbie Chippington Derrick
The Midwifery Unit Network, referred to as MUNet, was set up three years ago. They are a European group which focuses on Midwifery Led Units (MLUS) whether they are Freestanding Midwifery Units (FMUs) which are in a separate site to the hospital and Obstetric Unit (OU), or Alongside Midwifery Units (AMUs) which are on the same site as the Obstetric Unit. They are currently in the process of becoming a Community Interest Company (CIC) with a management team who will work closely with advisers from City University. MUNet’s mission is “To support and promote the development and growth of midwifery units (birth centres) throughout Europe, so they become the main care pathway for women with an uncomplicated pregnancy, providing holistic care to them and their families. To make midwifery units an easily accessible, mainstream option for women with uncomplicated pregnancies and their partners, through research, policy, leadership, quality improvement, training, influencing, information, support and networking activities.”
This conference was very well attended and presented the report of MUNet’s first three years’ achievements and they also launched their new Midwifery Unit Standards.1
Debra Salmon, Dean of School of Health, opened the meeting. Baroness Julia Cumberledge then began by talking about Continuity of Carer, giving the sad example of one woman who had previously lost a baby, who then had to tell the same story over and over again as she kept seeing different midwives at her antenatal appointments. Julia said that Continuity of Carer means a safer service. She also discussed working with NHS digital to put electronic notes on women’s devices with the aim of putting women more in control of their own care.
Sheena Byrom, MUNet Chair, reported on the first 3 years of MUNet. We were provided with a printed copy of the report (Midwifery Unit Network: the first three years) which is available from MUNet’s new website.1 Sheena talked about MUNet wanting birth centres to be the mainstream option for women, and not an add-on. She also said that MUNet are in the process of becoming a Community Interest Company (CIC).
Mary Ross-Davis, RCM Director for Scotland was up next. She spoke about the situation in Scotland where the key recommendation from the Scottish Maternity Review2 included a named obstetrician & link GP for each team of midwives. She talked about the huge variation in services across the country with differences for rural & urban people, affluent & poor, etc. Scotland’s homebirth rate is currently about 2.6%. Only six out of 18 OUs have a midwifery unit, but there are 19 FMUs. Changes of some OUs to midwifery units have not been positive as the changes were driven by a lack of staff, rather than because of any intended benefit for women. Some AMUs are currently closed due to staffing issues. There are no MLUs in the Glasgow area, despite this being where a significant proportion of the population live. Mary pointed out that one of the reasons that access to MLUs was limited is the very high induction rate, which is meaning that many women are then not eligible to give birth in them. In Scotland they are looking at changing guidelines on this issue although it was unclear whether this means fewer inductions rather than women who are induced being able to birth in the MLU.
Maria Healey of Queen’s University, Belfast, talked about the situation in Northern Ireland where there are five AMUs, three FMUs and one MLC (midwife led care). There are different access criteria for different units. They are working on improving guidelines for these units, as well as addressing the concern that women who were being referred for obstetric consultations were not returning to midwifery care when they should have been.
(AIMS have since found these link to the guidance which unfortunately does not fill us with confidence)
https://rqia.org.uk/RQIA/files/0b/0b9d5aee-0f80-47e6-8967-0c34216200af.pdf
And this link gives more background
www.rcm.org.uk/learning-and-career/learning-and-research/ebm-articles/planning-birth-in-and-admission-to-a-midwife
Cate Langley, Consultant Midwife, Hywel Dda University Health Board & Marie Lewis, Consultant Midwife, Powys Teaching Hospital Health Board, talked about what is happening in Wales where every OU has an AMU, and there are 10 FMUs. Powys has no OU, but 6 FMUs where 1400 women - 30% of women in Powys - start labour. Decisions about where to birth are made by women when they are in labour. Midwives manage their own time, and they do not have set working hours, which allows them to manage being on call for women. They don’t staff their birth centres, they staff the women! Cate talked about how midwives may be able to accompany women they are caring for when they go to the OU, although this isn’t always possible given a transfer time of up to 2 hours. 50% of women have a midwife they know in labour. Marie Lewis talked about the Powys midwives’ working patterns: No clinics, but individual appointments which can be cancelled and rebooked if a midwife is called to a birth.
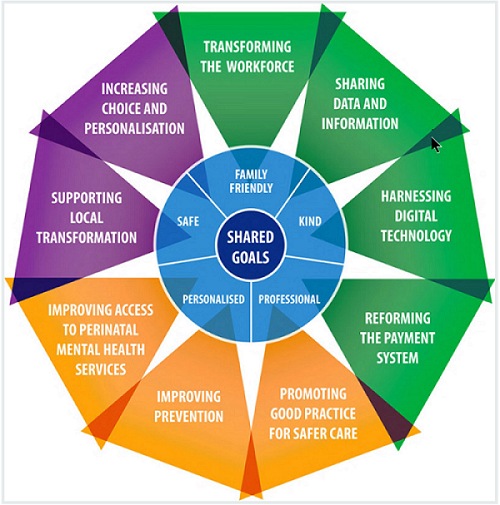
Matt Tagney, the Programme Director of the NHS England Transformation Board praised the Better Births report and those who had been involved in producing it. He went through the recommendations in Better Births, highlighting Continuity of Carer, MLUs and safety, and how ambitious the safety targets are. He talked about the nine workstreams in Better Births which can be seen in the diagram below and further information is available on the NHS England website, www.england.nhs.uk/mat-transformation
There is a decision aid for first time mothers3 and another for mothers of subsequent babies.4
Matt said that every area of the UK has provided NHS England with a plan to implement Better Births and claimed that that the CQC survey showed small, but significant positive changes. He stated that they had now achieved 9% continuity across London, but gave no further details about this, including what their definition of Continuity of Carer was. There are Community hubs which are beginning to link care around women, and he used the example of the new FMU in Salford. He did acknowledge that we still have a long way to go, that there are lots of challenges, but he said that he believes that the Continuity conversation has gone from ‘can we make it happen’, to ‘how can we make it happen’.
Birte Harlev-Lam, Clinical Director, Maternity and Children, NHS Improvement, talked about the aim to improve maternity services in 136 NHS trusts, and two providers of services from outside the NHS (Neighbourhood Midwives and One to One Midwives). Her talk was not directly related specifically to MLUs, but was more looking at improving maternity care overall.
Birth Centre Beacon Site Awards
Mary Newburn, Executive Manager, Midwifery Unit Network started by pointing out that a quarter (24%) of Trusts in England have no MLUs, and that there is a large variation in how many MLU births take place in different Trusts, from only 4% up to 31% of births. She said that only 1 in 6 Trusts have both an FMU and an AMU, and while the number of AMUs has doubled between 2010 to 2017, there has been no increase in the number of FMU.
She talked about the awards that MUNet were making and emphasised that they were looking for a philosophy of care, listing the criteria:
Awards were made to three units; Chorley & Preston, Halcyon & Serenity, and Lewisham.
Julia Cumberledge then introduced the award winners who each told us about the service they provide. She mentioned that one of the England football team had returned home because his wife was in labour with her third child – her third homebirth. She said that this could only happen when all the needs of a team member are being considered - crucial to building a strong and successful team.
The Award Winners:
Jo Goss, Matron for Midwifery-Led Services, Lancashire Teaching Hospital NHS Trust, gave a very lively talk about what they do well, including publicity. She said they have a diverse population, rural and urban, poor & affluent, different ethnic groups, etc. They have managed to get their FMU refurbished which has increased the birth rate there, and then developed an AMU. This is on the first floor, with the OU on a floor above, making it feel very separate. They have an integrated model with eight teams, covering homebirth and the MLUs. Last year their new staff were newly qualified midwives. They have individual plans for women who are making decisions that would not usually be recommended. She talked about training, multi-disciplinary work, networking, sharing learning and a supportive culture.
She was very clear that publicity can’t be underestimated. They establish and maintain communication with the potential “customers” by going out into the community and holding open days. They also work closely with other organisation and agencies.
Tracey Thomas, Lead Midwife, Lewisham and Greenwich HNS Trust, talked about the Lewisham Birth Centre starting by saying that although the building is beautiful, the team is the important part, and that many of the original core team still work there. When they recruit it is not only on the basis of clinical skill, but on philosophy too. They need a commitment to a shared goal and asked who would want to manage a team of “Stepford midwives”. She said that team work was essential and went on to explain that the midwives will not have met women before they come to the unit in labour, but their transfer rate is only 10% and 6% of women transfer for an epidural. What came over was that they are a team which not only works together, but they are also a social and supportive group.
Helen Giles, Midwifery Team Manager, Sandwell and Birmingham Hospitals NHS Trust, told us that Serenity Birth Centre has now been open eight years, and Halcyon’s seven year lease is coming to an end soon and the unit could be under threat. Helen said that when Kathryn Gutteridge first arrived at the Trust the Health care commission had said that they needed to improve, they had a caesarean rate of 37%, and induction rate of 43% and 15-20 complaints per month. The staff moral was low and they had a 15-20% midwifery vacancy rate. She said that they needed to ask “why would any decent midwife want to work here at the moment”. We have all seen the amazing midwifery unit that has come from out of the changes in Birmingham.
Helen also spoke about how they have redefined their criteria to include women with risk factors, with a positive focus on managing the risk. Women having a vaginal birth after a previous caesarean (VBAC), women with a BMI over 35, women with diet controlled gestational diabetes, women with hypothyroidism, a previous post partum haemorrhage (PPH), previous 3 and 4th degree tears, and previous retained placenta are not excluded. They have a guideline and a proforma for women planning a VBAC on the unit.
|
Sadly, despite the award made in July 2018, the Halycon was closed just three months later. The loss of the Halycon comes amid news of a number of other FMUs and AMUs which are being closed without proper consultation. Underuse is often quoted as a reason, but we know from enquires to the AIMS helpline that many women who want to birth in these units are being discourage or even refused access, and there is extensive feedback from local MSLCs that women are not being told by their community midwives that the option to birth outside the OU even exists. |
Lucia Rocca-Ihenacho, Lecturer in Midwifery and NIHR Research Fellow introduced the NICE Birthplace Action study, which is looking at the barriers and facilitators for the implementation of the NICE intrapartum guidelines recommendation on place of birth for women with uncomplicated pregnancies. Members of the research team spoke: Ellen Thaels, Research Fellow and Laura Batinelli, Research Midwife said that to make change you have to have an impact on hearts and minds. They talked about what they did to improve the environment in one unit, giving the whole team (including the cleaning staff) a practical challenge of making things look more homely and less medical. Before and after pictures were shown, which did show how much difference small changes could make. They looked at barriers and facilitators, and split work into workstreams to allow people to focus on a specific issue.
Lucia talked about the new Midwifery Unit Standards1, why they are important and what makes them work. They are rigorous, but inclusive with as wide an input as possible. There were stakeholder events and a systematic review of the literature, which only found 24 papers, and 3 PhD theses, and they interviewed those at Beacon sites. The twelve peer reviewers were also mentioned. Development challenges included gaps in evidence, how to rate different forms of knowledge and different terminology. There was a need for the standard to be applicable to countries who already have MLUs and those which don’t. She said that in translating the document to other languages it will be very important to maintain the core meanings of the guidelines.
Research Midwife Denis Walsh, who was in the audience, asked about the future of FMUs – given that the number of these is not growing. Research Midwife Chris McCourt pointed out they were superior in terms of outcomes for women and that there is a need to translate the economic evidence, as there is a false assumption that because it is attractive it must be expensive. Julia Cumberledge thanked Denis for all his work in this area and went on to talk about the need for all four places of birth to be available everywhere, and that this would also mean that pressure was taken off labour wards. Lucia talked about the potential for FMUs being the centres of care.
A midwife from Warrington FMU reminded us that FMUs are the safest place for women to have their first baby according to Birthplace5. This important outcome does seem to be being quietly swept under the carpet, and we probably do need to keep reminding ourselves that for low risk first time mothers the outcomes for their babies were the same whether they birthed in an OU, AMU or FMU, whilst rates of transfer, epidural, caesarean, assisted birth, episiotomy, blood transfusion and admission to higher level care were lower in FMUs compared to AMUs and OUs.
They announced that the next MUNet conference will take place in Barcelona in September 2019.
Dame Cathy Warwick closed the conference. She reflected on the day with “Wow, a fantastic day” and that you have to be prepared to run with the people who have ideas and enthusiasm. She said that she had been glad that in her position at the RCM she had been able to help in the early days, but that it was the ideas and enthusiasm that made it happen. She said that it was exciting to hear Matt Tagney say that we have to staff the women not the building, and that we need to think more creatively about staffing. She gave an example: In Fort William’s A&E, medical staff support the midwives. We need to be flexible and imaginative. She said that we had heard from academics, practitioners, policy makers, etc. and that there is a need to keep these different groups integrated, and that she really felt that this was coming through at this conference.
Julia Cumberledge concluded saying that MUNet should keep going, that they needed to make sure that they were well integrated alongside the other organisations working toward better maternity services and that she would like to see them do more about staffing and funding. But most of all to keep us motivated and thinking.
References
1. Midwifery Unit Network: The First Three Years: www.midwiferyunitnetwork.org/wp-content/uploads/PDFs/LY1308BRO-MUNEt-Three-Year-Report-PRINT-opt.pdf
2. Scottish Maternity Review: www.gov.scot/isbn/9781786527646
3. Decision aid for first time mothers: assets.nhs.uk/prod/documents/NHSE-your-choice-where-to-have-baby-first-baby-sept2018.pdf
4. Decision aid for mothers of second and subsequent babies: assets.nhs.uk/prod/documents/NHSE-your-choice-where-to-have-baby-baby-before-sept2018.pdf
5. Link to Birthplace https://www.bmj.com/content/343/bmj.d7400
The AIMS Journal spearheads discussions about change and development in the maternity services..
AIMS Journal articles on the website go back to 1960, offering an important historical record of maternity issues over the past 60 years. Please check the date of the article because the situation that it discusses may have changed since it was published. We are also very aware that the language used in many articles may not be the language that AIMS would use today.
To contact the editors, please email: journal@aims.org.uk
We make the AIMS Journal freely available so that as many people as possible can benefit from the articles. If you found this article interesting please consider supporting us by becoming an AIMS member or making a donation. We are a small charity that accepts no commercial sponsorship, in order to preserve our reputation for providing impartial, evidence-based information.
AIMS supports all maternity service users to navigate the system as it exists, and campaigns for a system which truly meets the needs of all.