To read or download this Journal in a magazine format on ISSUU, please click here
AIMS Journal, 2019, Vol 31, No 3
By Dr. Rehana Jawadwala

When we're pregnant, one of the easiest ways to put us off doing something is to tell us how our actions may have a negative impact on our unborn child. It’s the classic rabbit in the headlights. Fear, anxiety and lack of clear information can quickly elicit inaction.
When it comes to physical activity, moving more and generally enjoying our bodies whilst being pregnant, many women are terrified of placing a wrong foot forward… literally!
How helpful are official guidelines?
Reading the official guidelines, it’s not a surprise that some people are concerned. Some of the official guidelines are vague and unhelpful. They have more cautionary tones than encouragement. Keeping active throughout our pregnancies means we enjoy higher cardiorespiratory fitness, less chance of urinary incontinence (with low impact exercise) and less lower back pain. Physical activity also helps to lift depression. Fewer women who are diagnosed with gestational diabetes require insulin to manage their conditions when they are more active in pregnancy1. Compared to being sedentary, light to moderate activity is all that is required to reduce the incidence of preeclampsia by 24% (95% CI, 0.48 to 1.20)2.
But the benefits are not all for us, our unborn children have better protection against chronic non-communicable diseases such as obesity, diabetes and cardiovascular diseases when we exercise whilst being pregnant with them3.
And yet, this slow trickle of information and positive outcomes is not yet fully embraced by many midwives or consultants.
The National Institute for Clinical Excellence (NICE), for example has a rather vague statement on exercise during pregnancy. “Pregnant women should be informed that beginning or continuing a moderate course of exercise during pregnancy is not associated with adverse outcomes”4. This statement unfortunately does not encourage proactive action on trying to get more active and the benefits of doing so during pregnancy. In fact, the statement only points towards the lack of adverse outcomes. By simply mentioning that a particular activity will not have adverse outcomes does not encourage people into doing that activity, it may only increase anxiety about adverse outcomes. What adverse outcomes might there be? If you have not thought about adverse outcomes in relation to physical activity now you have a reason to worry. Stating that there will not be adverse outcomes also implies that women who like to do physical activity for themselves will not harm her baby - whereas instead we might be encouraged to consider all the benefits the baby will receive if we stay active during our pregnancy. This kind of advice gives very little incentive to women to start or continue exercising during pregnancy despite the benefits to them and their baby.
Not only does NICE give us this very vague and unhelpful statement, they actually go on to induce fear by mentioning all the things that may go wrong.
“Pregnant women should be informed of the potential dangers of certain activities during pregnancy, for example, contact sports, high-impact sports and vigorous racquet sports that may involve the risk of abdominal trauma, falls or excessive joint stress, and scuba diving, which may result in fetal birth defects and fetal decompression disease.”4
Just the long list of potential issues is enough to put off any responsible mother to be!
The information is not technically incorrect, but, like so many health warnings, such guidance suggests extraordinary levels of caution which can actually lead to women not wanting to do anything, just in case. It’s simply a matter of vocabulary. Using positive, empowering, clear and specific guidance is the way to encourage women to benefit from more physical exercise.
Simpler messages about reducing sedentary behaviour may be far more beneficial than talking about specific activities and their risks. These risks can be conveyed on a case by case basis or as caveats. The proportion of the pregnant population who may have a prior interest in contact sport or scuba diving is rather small! Why talk about these specific risks for extremely rare cases alongside the big and important message of staying active and reducing sedentary behaviour?
No time for exercise:
In preparation for this article, I put out a short survey within my network of mothers on social media. The survey asked several questions on barriers women faced during pregnancy towards getting and staying more active.
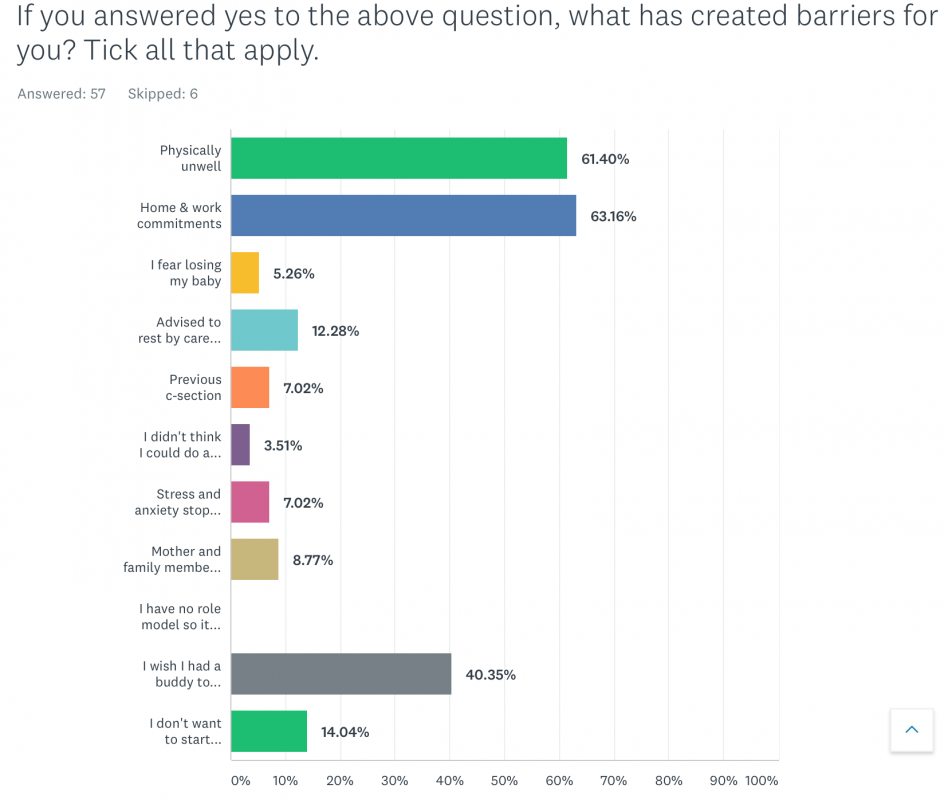
Out of this small snapshot of 57 respondents, 63% (n = 36) of them felt that their work and home commitments meant they gave less priority to physical activity. Could it be that without guidance from our midwife clearly stating the benefits of moving more during pregnancy (light to moderate physical activity) we don’t prioritise our valuable time to make sure we include it?
Role of health care providers:
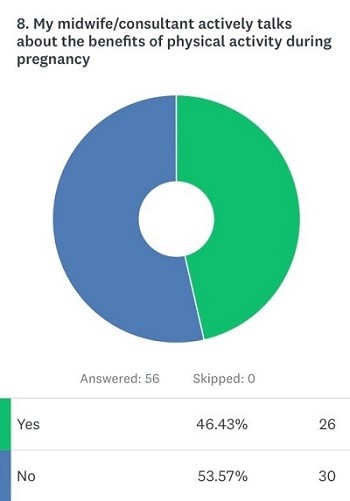
Healthy eating advice is a routine part of antenatal care, yet physical activity is not addressed with the same enthusiasm. Almost 54% of our respondents said their care providers did not actively talk about exercise and movement during pregnancy.
A recent study5 conducted as semi-structured interviews with midwives, have identified lack of resources specifically designed to encourage women to take up exercise during pregnancy. One midwife responded, “…I can’t think of any Trust or NHS leaflets specifically about exercise where there is on diet, there is on drinking, there’s on smoking.”
Other factors play a role in discussions on physical activity during pregnancy too. In the same study the midwives who were interviewed identified a lack of specific knowledge and training on giving advice and guidance to the people in their care. They also said that physical activity is only a tick box for the booking appointment and there are no recurring prompts to discuss the agenda throughout antenatal care. Some of the more insidious reasons the midwives stated for not talking about an active pregnancy included fear of litigation, high workload and their own personal beliefs.
For example, one of the interviewees said, “I don’t think a pregnant woman is going to start exercising because she is pregnant necessarily”. This sort of personal bias belief will only serve to further alienate the topic and not help women to feel confident about starting or continuing to be active during her pregnancy months.
Health related barriers:
Of 57 responses to this question, more than 61% (n=35) of our respondents stated health related issues such as lack of energy, back ache and general nausea as their reason for reduced physical activity. Ironically these are all known to be helped by physical activity6. A larger survey7 agrees that health related barriers are a major determinant in lower participation of physical activity among pregnant women. Among the 1535 pregnant women participating in the survey, 85% reported barriers such as feeling judged for having a high BMI, health conditions such as diabetes or other restrictions such as childcare issues and lack of motivation were all important aspects in reducing physical activity.
The question, then, is how to facilitate an increase in physical activity if we suffer from physical discomfort during exercise? When a study8 looking at increasing physical activity levels among overweight and obese pregnant women examined ways of encouraging the participants to increase their levels of physical activity, they found using mind-maps and identifying individual barriers and enablers (things the women considered helpful in doing physical activity) were an important aspect of making changes to our behaviour and practices. But even more importantly, what are barriers to some of us are actually enablers to others. For example, a high BMI or gestational diabetes can be a major barrier to exercise for many and yet it can become a source of motivation for some.
Despite there being various reasons people cite for not being able to do more physical activity, it is important to understand reasons that are specific to each individual. For some, the lack of affordable childcare means we cannot engage in certain activities despite having the motivation and desire to do so. For others, it’s the intrinsic motivation that needs addressing. So, each one of us will have valid reasons which reduces our ability and participation in physical activity. Thus, the solution has to be one that considers individual circumstances rather than a “package” that is rolled out without nuanced understanding of why we struggle to keep active during pregnancy. Hopefully, this individualised need, driven by us, will encourage guidelines to be more positive, encouraging and appropriate. This in turn will empower midwives, who will be at the forefront of supporting women to seek the training to help to provide this individualised care.
But with the current vague official guidelines, extra cautionary tones and lack of care providers’ engagement with building evidence of the benefits of physical activity during pregnancy, it is an uphill battle to increase the sense of priority to exercise during pregnancy.
Women’s desire to move more:
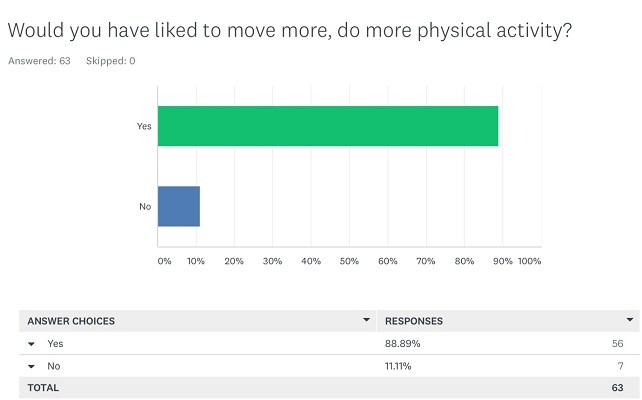
Despite setting lower priority to physical activity during pregnancy, a staggering 89% (n=56) of the respondents in our survey said they would like to do more exercise.
The barriers to physical activity are a real and important part of this conversation. The physical discomfort of moving, the lack of access to other pregnant women within our community, social pressures to “take it easy”, childcare and other financial burdens all contribute towards lower physical activity.
Make it social:
In my survey of 57 responses just over 40% (n=23) highlighted the need to find a likeminded “buddy” to exercise. This social aspect of physical activity has been shown in research9 as an important benefit for not only increased commitment to physical activities but it also improves our mental health. Further research10 indicates that inactivity during pregnancy worsened mood amongst pregnant women. Part of the mood enhancing effects of having an exercising buddy are the social connections we build.
Creating a culture of shared physical activity amongst pregnant women helps us in creating deep bonds. The natural law of coupled oscillators holds that when two or more rhythms meet, they will become coordinated—a phenomenon seen across the natural world, from fireflies matching their flashes to groups falling into step. There is some evidence beginning to gather that bodily movement, such as communal dancing, allows for heart rates to synchronise and thus increase empathy and bonding between members of the same group11. The bonding that doing physical activity together creates, allowing us to be in a positive mental space during pregnancy, can help create strong networks of new mothers within our community.
What can we do?
As a first step we need to have more robust ways to document the current levels of physical activity of pregnant women, so we have a good idea of what the current situation is. There is very little research on profiling the physical activity levels of women during pregnancy. We have no idea what the picture is nationally and if there are any pockets of good practice in the country where we can call upon the success of those ideas to inform a good, structured and coherent strategy on getting the message of physical activity louder.
We need a strategy where we see physical activity conversations between pregnant women and care providers to be more than a tick-box exercise. There needs to be an increased awareness of this from our midwives and as we demand more meaningful conversations, resources and guidance we can hope that this will translate to better training for the care providers too. Better training will mean that the midwives and other carers in pregnancy will not feel intimidated by our requests but will be sufficiently equipped to answer our questions.
The language that is used is key. We must consider the impact of vocabulary. A positive approach rather than the cautionary words about sports that most of us will never do are more likely to create engagement with physical activity across our entire pregnancy journey.
Midwives and other care providers need more training and support in talking to women about the health aspects of exercise. We have strategies for smoking reduction, healthier eating and other positive health messages. We don’t say that eating more vegetables won’t have a negative impact on ourselves and our baby! Why are we saying the same thing with exercise?
We definitely need a clear and loud message. We don’t expect to complete physically challenging activities like running marathons without any physical and mental training. We as a society have even started to grasp the importance of preparing mentally and building emotional resilience to encounter the event of birthing our babies. And yet, we are reluctant to talk about the need to physically keep strong, active and prepare for birth which is one the most physically demanding activities we as women will ever do. But we know that an active pregnancy is not only about birth, it’s about the resilience of the next generation3, it is about combating lifestyle generated diseases in our future generations, it is about changing our epigenetic profile during pregnancy to improve the quality of life for not only our children but our grand and great grandchildren!
Let’s talk about moving more during pregnancy… all of us; pregnant women, our care providers and society at large.
References:
1. Nascimento SL, Surita FG, Cecatti JG. Physical exercise during pregnancy. Curr Opin Obstet Gynecol. 2012;
2. Sorensen TK, Williams MA, Lee IM, Dashow EE, Thompson M Lou, Luthy DA. Recreational physical activity during pregnancy and risk of preeclampsia. Hypertension. 2003 Jun 1;41(6):1273–80.
3. Moyer C, Reoyo R, May L. The Influence of Prenatal Exercise on Offspring Health: A Review. Clin Med Insights Women’s Heal [Internet]. 2016 [cited 2018 Jun 16];9–37. Available from: www.ncbi.nlm.nih.gov/pmc/articles/PMC5075987/pdf/cmwh-9-2016-037.pdf
4. NICE. Antenatal care for uncomplicated pregnancies. Clin Guidel [CG62] [Internet]. 2008 Last updated: February 2019; Available from: www.nice.org.uk/guidance/cg62
5. Marlize De Vivo & Hayley Mills. “They turn to you first for everything”: insights into midwives’ perspectives of providing physical activity advice and guidance to pregnant women. Sport Rxiv [Internet]. 2019; Available from: https://scholar.google.co.uk/scholar?cites=8340366314463355019&as_sdt=2005&sciodt=0,5&hl=en
6. Nascimento SL, Surita FG, Cecatti JG. Physical exercise during pregnancy: A systematic review. Current Opinion in Obstetrics and Gynecology. 2012.
7. Evenson KR, Moos MK, Carrier K, Siega-Riz AM. Perceived barriers to physical activity among pregnant women. Matern Child Health J. 2009;
8. Sui Z, Dodd JM. Exercise in obese pregnant women: Positive impacts and current perceptions. International Journal of Women’s Health. 2013.
9. Coll CVN, Domingues MR, Gonçalves H, Bertoldi AD. Perceived barriers to leisure-time physical activity during pregnancy: A literature review of quantitative and qualitative evidence. Journal of Science and Medicine in Sport. 2017.
10. Poudevigne MS, O’Connor PJ. A review of physical activity patterns in pregnant women and their relationship to psychological health. Sports Medicine. 2006.
11. Reddish P, Fischer R, Bulbulia J. Let’s Dance Together: Synchrony, Shared Intentionality and Cooperation. PLoS One [Internet]. 2013 Aug 7;8(8):e71182. Available from: https://doi.org/10.1371/journal.pone.0071182
The AIMS Journal spearheads discussions about change and development in the maternity services..
AIMS Journal articles on the website go back to 1960, offering an important historical record of maternity issues over the past 60 years. Please check the date of the article because the situation that it discusses may have changed since it was published. We are also very aware that the language used in many articles may not be the language that AIMS would use today.
To contact the editors, please email: journal@aims.org.uk
We make the AIMS Journal freely available so that as many people as possible can benefit from the articles. If you found this article interesting please consider supporting us by becoming an AIMS member or making a donation. We are a small charity that accepts no commercial sponsorship, in order to preserve our reputation for providing impartial, evidence-based information.
AIMS supports all maternity service users to navigate the system as it exists, and campaigns for a system which truly meets the needs of all.