AIMS Journal, 2025, Vol 37, No 4

By Pavithra Harshani Warnakulasooriya and Mairead Black
Access to safe, timely, and coordinated maternity care is a cornerstone of healthy pregnancy outcomes. Yet, for many women, particularly those with pre-existing multiple long-term conditions (MLTCs, otherwise referred to as multimorbidity), geographic, socioeconomic, and systemic barriers can create substantial challenges in receiving adequate care. In high-income countries, centralisation of maternity services has often been implemented to improve clinical safety and ensure access to specialist staff. While this model may enhance neonatal outcomes in high-volume centres, it can inadvertently increase travel distances for women who require frequent and multidisciplinary care, disproportionately affecting those with complex health needs.1
Evidence from multiple settings demonstrates that travel distance is more than a logistical concern; it has potential to influence maternal and neonatal outcomes, exacerbate psychosocial stress, and compound existing inequities. Longer journeys to hospitals are associated with increased risks of babies being born before reaching the hospital, delayed interventions, and poorer adherence to antenatal care. Vulnerable populations, including first-time mothers, women living in rural or deprived areas, and those with MLTCs, face compounded risks, as structural factors such as urban deprivation, limited transport options and fragmented care pathways intersect with the challenges of distance (Malouf et al., 2020a).2
This article examines the impact of travel barriers on perinatal outcomes and maternal well-being, drawing on quantitative population-based studies and qualitative research from a range of high-income countries, including the UK and the Netherlands. By synthesising evidence on neonatal mortality, maternal morbidity, service centralisation and lived experiences of women with complex health needs, the review highlights how geographic access, systemic inequities, and fragmented care intersect to shape pregnancy outcomes. The findings underscore the need for policy approaches and service models that address travel-related barriers, provide equitable access to specialist care and support person-centred pathways for high-risk populations.
A qualitative study of pregnancy care of women with MLTCs revealed that care was often fragmented, insufficiently individualised and managed by clinicians with limited expertise in pregnancy care. These systemic gaps contributed to negative outcomes, including heightened psychological distress (Hanley et al., 2024).3
A major theme emerging from the lived experiences of these women is the burden of “responsibilities”, where women must act as the primary coordinators of their care, navigating between primary care, speciality services, and maternity teams.3 Many described feeling isolated, overwhelmed, and unsupported by disjointed care systems. When healthcare teams failed to communicate or lacked a unified plan, women were left with the task of reconciling conflicting clinical advice, often at the expense of their confidence and well-being. This burden became even greater when access to care was affected by geographical constraints.
Travel is a critical but often underestimated barrier in the maternity care of women with complex needs. Malouf et al. (2020)2 systematically reviewed 31 studies from high-income countries with universal healthcare coverage. They found that longer travel times and distances to obstetric units were associated with a higher incidence of babies born before arrival. This is a clinically significant event that may be linked to increased perinatal and neonatal mortality. Although the evidence was less conclusive for other maternal and neonatal outcomes, the review identified travel delays as a plausible risk factor for adverse outcomes, particularly in emergencies (Malouf et al., 2020).2
Further, recent evidence from Northern Ireland underscores how structural inequalities, including geographic and socioeconomic disparities, intersect with maternal multimorbidity. To assess the prevalence and patterns of pre-existing multimorbidity in pregnancy in Northern Ireland, Kent et al. (2025)4 found that women from the most deprived areas had higher rates of multimorbidity and obesity (obesity being a marker for an increased incidence of multimorbidity) and were more likely to live in rural or intermediate settlements. These women may face compounded barriers in accessing timely and coordinated maternity care, with the Northern Ireland multiple deprivation measure explicitly recognising “access to services” as a domain of deprivation. Such findings highlight how travel-related challenges are not uniformly distributed but are shaped by where women live, their socioeconomic status, and their health complexity (Kent et al., 2025).4 The centralisation of maternity care services as a strategy, intended to improve clinical safety and consultant cover (the ready availability of a consultant on site), has led to the closure of smaller, local obstetrics units and a shift toward larger regional facilities. While this model may enhance access to specialist care for some, it disproportionately affects women with MLTCs who require frequent and multidisciplinary input. The need to travel greater distances for specialised services can be especially burdensome for those already managing comorbidities, disability, or psychological distress (Hanley et al., 2024; Malouf et al., 2020).3, 2
Moreover, travel exacerbates emotional stress when it delays timely access to critical services. In Hanley’s qualitative study, several women described feeling like a ‘ticking time bomb’ due to the absence of coordinated care early in pregnancy. Many reported that care only became cohesive after they were referred to distant specialist centres. The emotional toll of travelling to unfamiliar hospitals, often after previous traumatic births, contributed to feelings of mistrust, fear, and disempowerment (Hanley et al., 2024).3
The potential association between travel time to maternity services and adverse birth outcomes is further supported by a population-based study in Wales analysing data from 412,827 singleton births (1995–2009) by Paranjothy et al. (2014).5 The study found that for every 15-minute increase in travel time to the birth hospital, there was a statistically significant increase in the risk of early and late neonatal death.6 Specifically, early neonatal deaths occurred in 0.4% of births closest to the hospital compared with 0.5% for those furthest away. In comparison, late neonatal deaths occurred in 0.2% of births closest to the hospital versus 0.3% furthest from the hospital. Evidence regarding intrapartum stillbirth was inconclusive, showing no clear pattern. Importantly, the study distinguished between travel time to the birth hospital and proximity to the nearest maternity unit. While longer travel to the birth hospital was linked to poorer outcomes, proximity to the nearest hospital alone did not show a significant association with overall adverse outcomes, suggesting that outcomes may depend more on the quality of neonatal transfer systems than on geographic access alone (Paranjothy et al., 2014).5 This aligns with Malouf et al.’s (2020)2 systematic review, which emphasised the importance of timely transfers in reducing risks associated with centralisation. Subgroup analyses revealed that vulnerable groups—especially first-time mothers—were most affected. Longer travel times were linked to higher risks of intrapartum stillbirth and early neonatal death, underscoring the compounded risks faced by women with limited childbirth experience. This is consistent with Hanley et al.’s (2024)3 observations that fragmented care can increase stress for high-risk groups. The Welsh study concluded that while centralisation does not inherently worsen outcomes, equitable access depends on robust neonatal transport services and localised resuscitation capabilities (Paranjothy et al., 2014).5 This is consistent with the findings of Kent et al. (2025),4 who noted that geographic deprivation, especially among women with multiple health conditions in rural or deprived areas, can exacerbate risks.
The association between travel barriers and adverse perinatal outcomes is well-documented in high-income countries with different healthcare systems. In the Netherlands, where many low-risk pregnancies begin with planned home births, Ravelli et al. (2011)7 found that term pregnancies with travel times of 20 minutes or more to a hospital faced a small but statistically significant increased risk of intrapartum or early neonatal death. For example, early neonatal deaths occurred in 0.3% of births closest to the hospital compared with 0.5% of those furthest away, and deaths within the first 24 hours were notably higher among those living further from hospitals. These risks were even greater for women whose pregnancies shifted from low- to high-risk during labour, highlighting the dangers of delayed access to emergency care. Similarly, Paranjothy et al. (2014)6 reported that longer travel times in Wales were associated with higher neonatal mortality, though strong neonatal transfer systems helped reduce the impact of geographic distance. Both studies support Malouf et al.'s (2020)2 systematic review, which showed that longer distances to obstetric units increased the likelihood of babies being born before reaching the hospital, which is a key indicator of limited healthcare access. The Dutch study highlighted how structural factors, such as living in rural areas, can intensify the risks associated with travel. Hanley et al. (2024)3 further demonstrated the psychological stress and complications faced by women with multiple health conditions when care pathways are fragmented. Together, this evidence shows that travel time is more than a logistical concern; it is a critical factor in ensuring equitable perinatal outcomes, particularly for high-risk populations such as women with MLTCs. The evidence calls for tailored solutions in both centralised and decentralised maternity systems.
Pilkington et al. (2014)8 analysed 3.1 million births in France (2001–2008) to examine the impact of maternity unit closures and travel distances on perinatal mortality in France. Contrary to expectations, adjusted models revealed no significant association between distance to the nearest maternity unit and stillbirth or neonatal mortality rates, except for rare out-of-hospital births. However, women living 45 km or more from the hospital had substantially higher rates of complications and adverse birth outcomes than those living closer, 1.5% compared with 0.4%; but interestingly, the highest neonatal mortality rates were observed among women living very close to maternity units (less than 5km), where around 0.6% of newborn babies died.
This paradox is thought to result from concentrations of urban deprivation, including higher unemployment and larger immigrant populations, which independently contribute to poorer outcomes. This aligns with Grzybowski, Stoll and Kornelsen's (2011)9 findings in rural Canada but contrasts with Ravelli et al.'s (2011)7 Dutch cohort, highlighting how structural inequities (socioeconomic deprivation, access barriers for marginalised groups) often outweigh geographic distance as determinants of perinatal risk. The Pilkington study challenges assumptions that centralisation improves outcomes, highlighting the need for more targeted interventions in high-risk urban areas as a priority instead. This conclusion resonated with those who stated that person-centred care models address systemic fragmentation (Pilkington et al., 2014).8
Koller et al., (2024)10 in Germany showed that of all births, 53.1% occurred in perinatal centres, and 7.3% in regional hospitals with less than 500 births per year. The travel distance to higher level perinatal centres11 (L1 and L2) was slightly longer (16.0 km) than to the other hospitals (11.2 km). Mothers who chose the closest hospital travelled an average distance of 9.1 km, while women who chose a more distant hospital (n=95,475, 48.9%) travelled an average of 22.1 km. These scholars highlighted the influence of geographic distance on hospital choice for childbirth, with women in rural areas facing longer travel distances to access perinatal centres. The study underscores that while many women prioritise proximity, those in remote regions must travel significantly farther, potentially compromising timely access to specialised care.
Cantarutti et al. (2025)12 in Lombardy, Italy, examined the impact of hospital maternity unit volumes (the number of babies born each year in each unit) and road travel distance on neonatal outcomes, revealing critical insights into how travel barriers may indirectly affect maternal care. While the primary focus was neonatal outcomes, the study found that longer travel distances were associated with lower adherence to antenatal care,13 a key determinant of maternal health. Specifically, women travelling ≥15 km to hospitals had reduced adherence, which could delay the detection and management of pregnancy complications, particularly for those with multimorbidity. Although the study did not directly link road travel distance to adverse maternal outcomes, the disruption in antenatal care continuity underscores how geographic barriers may exacerbate risks for high-risk pregnancies by limiting timely access to preventive and specialised care. These findings align with broader evidence that centralising maternity services, while beneficial for neonatal outcomes in high-volume centres, may inadvertently strain maternal health systems by imposing travel burdens on vulnerable populations.
The study by Kornelsen and Grzybowski (2004)14 highlights the profound physical, emotional, and financial burdens on women in remote British Columbia communities, who must travel long distances to give birth due to the lack of local maternity services. Their qualitative research reveals that forced evacuation to referral centres creates significant psychosocial stress, particularly for indigenous women who experience cultural dislocation from traditional community-based birthing practices. Women reported anxiety from being separated from family support systems, with mothers especially distressed about leaving older children behind. The financial costs of extended stays in referral communities, including uncovered expenses for food, communication, and childcare, compounded this stress, while non-indigenous women faced additional inequities in travel reimbursement. These travel-related burdens were linked to health effects, including increased smoking, loss of appetite, loneliness, worry, anxiety. The study underscores how systemic healthcare service centralisation disproportionately affects rural women, creating a cascade of negative consequences that extend beyond clinical outcomes to include cultural erosion and community fragmentation.
The impact of service centralisation on rural populations in Canada is starkly illustrated by Grzybowski, Stoll and Kornelsen (2011), who analysed 49,402 singleton births in rural British Columbia (2000–2004). Their study revealed a threefold increase in perinatal mortality for women living >4 hours from maternity services with caesarean capability, alongside elevated NICU admissions (179 days per 1,000 births for those 2–4 hours away vs. 42 days for urban counterparts). Notably, logistical challenges such as unplanned out-of-hospital deliveries and inductions to mitigate travel burdens disproportionately affected rural women, particularly indigenous and socioeconomically vulnerable groups.
These findings align with Ravelli et al. (2011)7 and Pilkington et al. (2014)8 in demonstrating how distance exacerbates structural inequities and health disparities, particularly for vulnerable populations managing complex pregnancies or multimorbidity in resource-limited settings. These studies highlight the need to weigh the costs of service closures (additional NICU expenditures, psychosocial stress) against purported efficiencies of centralisation, advocating for context-sensitive maternity care models in remote regions. Addressing these barriers requires systemic improvements in service distribution and targeted support, such as travel subsidies, community-based care options, and culturally appropriate services that reduce the need for disruptive relocations during pregnancy.
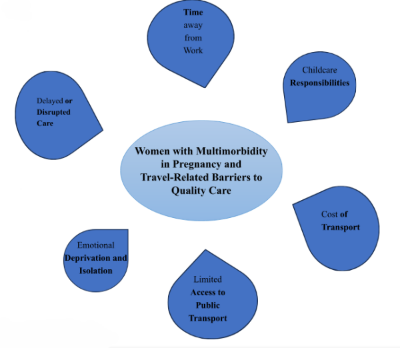
The themes that emerged from the studies include:
Time away from Work - Frequent medical appointments and travel time disrupts employment, resulting in loss of income or use of unpaid leave, which can be especially detrimental for women in insecure or low-paid work.
Childcare Responsibilities - Arranging childcare for existing children to allow travel and attendance at maternity care or specialist appointments adds emotional and financial strain; especially for single parents or those without extended family support.
Cost of Transport - Travel to distant hospitals or specialist centres incurs out-of-pocket expenses for fuel, public transport, parking, and sometimes overnight stays. These costs disproportionately affect low-income families and those in rural areas.
Limited Access to Public Transport - In remote or underserved areas, inadequate transport options reduce timely access to emergency and routine care, contributing to missed appointments and fragmented antenatal care.
Emotional Deprivation and Isolation - Long journeys to unfamiliar hospitals, often after traumatic past experiences, intensify feelings of fear, disempowerment, and stress; especially in the absence of a clear, coordinated care plan.
Delayed or Disrupted Care - Centralised services mean that women with complex needs must travel further for multidisciplinary care, which has been linked to complications due to delays in diagnosis, referral, or intervention.
Travel is not just a logistical inconvenience for women with multimorbidity during pregnancy; it is a structural barrier with measurable effects on access, safety, and outcomes. When layered onto a backdrop of fragmented service delivery, the impact of travel further limits these women’s ability to receive equitable, high-quality, person-centred care. Addressing this issue will require re-evaluating how maternity services are distributed and integrated, particularly for those managing complex needs across wide geographies.
Author Bios:
Mairead Black is a Reader and Honorary Consultant Obstetrician at the University of Aberdeen.
Pavithra Harshani Warnakulasooriya is an Honorary Research Fellow at the Foresterhill Campus and Hospital, University of Aberdeen.
1Koller, D., Maier, W., Lack, N. et al. Choosing a maternity hospital: a matter of travel distance or quality of care?. Res Health Serv Reg 3, 7 (2024). https://doi.org/10.1007/s43999-024-00041-1
2 Malouf, R.S. et al. (2020) ‘Impact of obstetric unit closures, travel time and distance to obstetric services on maternal and neonatal outcomes in high-income countries: A systematic review’, BMJ Open, 10(12), pp. 1–41. doi:10.1136/bmjopen-2020-036852. https://bmjopen.bmj.com/content/bmjopen/10/12/e036852.full.pdf
3 Hanley, S.J. et al. (2024) ‘Lost in the System: Responsibilisation and Burden for Women With Multiple Long-Term Health Conditions During Pregnancy’, Health Expectations, 27(3). doi:10.1111/hex.14104. https://pmc.ncbi.nlm.nih.gov/articles/PMC11176589/#Lost in the System: Responsibilisation and Burden for Women With Multiple Long‐Term Health Conditions During Pregnancyhex14104-bib-0006
4 Kent, L. et al. (2025) ‘Prevalence and patterns of pre-existing multimorbidity in pregnancy in Northern Ireland: a population-based, retrospective study using linked routinely collected healthcare data’, BMC Pregnancy and childbirth, 25(1), p. 666. doi:10.1186/s12884-025-07771-1. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-025-07771-1
5 Paranjothy, S. et al. (2014) ‘Perinatal outcomes and travel time from home to hospital: Welsh data from 1995 to 2009’, Acta Paediatrica, International Journal of Paediatrics, pp. e522–e527. doi:10.1111/apa.12800.
6 Editor’s note: Early neonatal death occurs during the first 7 days after the birth, while late neonatal death occurs between days 8 and 28 after the birth.
7 Ravelli, A.C.J. et al. (2011) ‘Travel time from home to hospital and adverse perinatal outcomes in women at term in the Netherlands’, BJOG: An International Journal of Obstetrics and Gynaecology, 118(4), pp. 457–465. doi:10.1111/j.1471-0528.2010.02816.x. https://pure.rug.nl/ws/portalfiles/portal/2515849/Ravelli_2011_BJOG.pdf
8 Pilkington, H. et al. (2014) ‘Where does distance matter? Distance to the closest maternity unit and risk of foetal and neonatal mortality in France’, European Journal of Public Health, 24(6), pp. 905–910. doi:10.1093/eurpub/ckt207. https://shs.hal.science/halshs-01010272/file/ckt207.pdf
9 Grzybowski, S., Stoll, K. and Kornelsen, J. (2011) ‘Distance matters: A population-based study examining access to maternity services for rural women’, BMC Health Services Research. doi:10.1186/1472-6963-11-147. https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-11-147
10 Koller, D. et al. (2024) ‘Choosing a maternity hospital: a matter of travel distance or quality of care?’, Research in Health Services & Regions, 3(1), pp. 1–8. doi:10.1007/s43999-024-00041-1. https://link.springer.com/article/10.1007/s43999-024-00041-1
11 Editor’s note: In the Koller study, the level of care available in different maternity hospitals was categorized in levels L1 to LVI (1-6), with L1 representing the highest level of care to L6 with the least provision of care.
12 Cantarutti, A. et al. (2025) ‘Assessing the Impact of Distance Travelled and Birth Volumes of Hospital Maternity Units on Newborn Outcomes: Population-Based Cohort Study’, JMIR Public Health and Surveillance, 11. doi:10.2196/58944. https://publichealth.jmir.org/2025/1/e58944
13 Editor’s note: The term ‘adherence to antenatal care’ is defined, in the study cited, in terms of the mother’s compliance with the hospital’s schedule of appointments, scans and tests. Antenatal ‘surveillance’ may be a more accurate word than ‘care’ in this respect.
14 Kornelsen, J. and Grzybowski, S. (2004) ‘The costs of separation: The birth experiences of women in isolated and remote communities in BC’, Canadian Woman Studies, 24(1), p. 75. https://med-fom-crhr.sites.olt.ubc.ca/files/2012/02/thecostsofseparation.pdf
The AIMS Journal spearheads discussions about change and development in the maternity services..
AIMS Journal articles on the website go back to 1960, offering an important historical record of maternity issues over the past 60 years. Please check the date of the article because the situation that it discusses may have changed since it was published. We are also very aware that the language used in many articles may not be the language that AIMS would use today.
To contact the editors, please email: journal@aims.org.uk
We make the AIMS Journal freely available so that as many people as possible can benefit from the articles. If you found this article interesting please consider supporting us by becoming an AIMS member or making a donation. We are a small charity that accepts no commercial sponsorship, in order to preserve our reputation for providing impartial, evidence-based information.
AIMS supports all maternity service users to navigate the system as it exists, and campaigns for a system which truly meets the needs of all.