To read or download this Journal in a magazine format on ISSUU, please click here
AIMS Journal, 2017, Vol 29 No 4
How they come about, and what you might expect when you’re expecting them
By Rebecca Freckleton
Finding out that you are expecting multiples is a special moment and often something of a surprise. Once the fog begins to clear, questions about the type of twins you are carrying and what this might mean for the journey ahead can begin to shape your thinking and inform your choices for pregnancy and birth.
There are several different types of twins - some are very rare and scientifically fascinating, others more common but equally intriguing. The general public will always ask if your twins are identical and healthcare providers prioritise determining chorionicity (the number of placentae accompanying the babies) at the earliest opportunity - so everyone will have an interest in what type of twins you are having. During pregnancy, the type(s) of multiples a woman is expecting can make a big difference to her experience, so it is useful to know this information. Finding out the type of multiples you are carrying will help you know how your babies came to be, what antenatal care you might expect and want to choose, and what multiple specific experiences you could encounter during your pregnancy and birth.
The aim of this article is to define different types of multiples, the common and medical terms used to describe them and how this might impact on your pregnancy and birth decisions.
Identical or Non-Identical?
When you have young twins in your family, people will invariably ask ‘are they identical?’ This is more a fascination held by the general public than healthcare providers, as in itself it is not an indicator for specific health advice. Being identical or not depends on the babies’ zygosity; that is how many fertilised eggs (zygotes) they develop from. A single zygote can divide to develop into two, or very rarely three, separate monozygotic embryos leading to identical multiples. When multiple eggs are released and fertilised separately (or implanted during fertility treatment) they lead to embryos that are dizygotic (from two zygotes) or trizygotic (from three zygotes). These multiples are referred to as fraternal and are no more ‘identical’ than singleton siblings.
Identical multiples
Identical multiples originate from 1 fertilised egg (monozygotic). The egg is fertilised by 1 sperm and then splits within the first couple of weeks of development. These identical babies share the same DNA from their genetic parents and so have an identical genetic make up. About 30% or 1 in 3 sets of twins are identical (1),(2).
For identical twins, the point in time at which the egg cleaves or splits after fertilisation will determine whether the babies share a placenta, an amniotic sac or both. An egg which divides within the first 72 hours will result in twins each with their own placenta and amniotic sac. This accounts for around 20% - 30% of identical twins (3),(4). Division at 3 - 8 days (around 60% - 70% of identical twins) will typically result in twins sharing a placenta but each with their own amniotic sac (5). At 8 - 12 days, an egg cleaving (splitting) will result in identical babies that will grow together in a single amniotic sac and share a placenta. Twinning occurring beyond 12 days could lead to conjoined twins, where babies share, to varying degrees, parts of their bodies. Twinning beyond 8 days is rare and represents about 1% of all twins (6).
Mirror twins are a subset of monozygotic twins, usually resulting from a zygote dividing between 9 and 12 days. They display mirrored physical attributes such as one being right-handed and one left-handed; birthmarks, dental structure and hair partings may also be in mirror image for this particular group of identical twins. In some cases internal organs may also be arranged in mirror image and this is called situs inversus. This is not deemed to cause any notable medical complications for those individuals with the condition, but it is useful for families and individuals to be aware so as to pass on to any services who may need to know in the future (7)
Identical twins resulting from an early egg division, which therefore have their own placentae, can only be verified as identical from a DNA test post-birth. Identical twins will share a common blood group, have the same skin, hair and eye colour, be of the same gender and look very similar. If twins seem identical but each had their own placenta it might be useful for the parents to find out about taking DNA tests for the babies if they would like verification.
Twins being of different gender is taken as clinical proof that they are not identical. Identical twins have to be of the same sex to share the same DNA. However, it can happen that monozygotic twins present as a boy / girl pair. Eggs usually carry a pair of XX chromosomes and contribute one of these to the zygote that forms, the sperm offers up the other chromosome, X or Y determining the baby’s gender. In very rare instances an egg will have an extra chromosome, which can develop into a zygote with XXY chromosomes. If this zygote then divides, creating twins, different chromosomes may be dropped by each embryo, leaving an XX female embryo and an XY male embryo. Because chromosomes make up our DNA and, in this instance, these are changed during the cleaving process, these twins would not be truly identical but do come from the same egg so are monozygotic. Only a handful of these cases are known, it is extremely rare (8).
Half-identical twins
There is a theory that an egg may split before fertilisation and that two different sperm can create separate embryos. For these ‘half-identical’ or ‘polar body twins’ the DNA match would be closer to 75%, as they inherit different genes from their father but share their mother’s (9).These babies would have separate placentae as the egg has already split before fertilisation. Half-identical twins would not be as similar as identical twins but share more similarities than the ‘average’ sibling.
Non-identical multiples
Non-identical multiples (usually referred to as fraternal) result from separate eggs and separate sperm. These babies are as genetically linked to each other as any singleton siblings (with on average a 50% DNA match), but are usually conceived at the same time and carried in-utero together. These babies will each have their own amniotic sac and placenta. These are the most common type of twin and account for around ⅔ of all twins or 7 out of 10 sets of twins(2),(10).
Very occasionally, non-identical twins can be conceived at different times, either within the same menstrual cycle (superfecundation) or much more rarely as a result of an egg being released during pregnancy (superfetation). This can lead to the possibility of non-identical twins having different fathers and being half-siblings (10). Twins conceived at different times will still be born together, but at different gestation, and therefore possibly have different medical needs.
More than two
Triplets and more can be made up solely of non-identical babies, or a combination of identical and non-identical babies, eg two eggs fertilised separately, one of which goes on to divide could lead to triplets including a pair of identical twins and one non-identical twin. Very rarely identical triplets can occur where the egg splits twice after fertilisation to create three separate embryos.
Chorionicity & Amnionicity
Healthcare providers will refer to twin types by their chorionicity and amnionicity and define their recommended antenatal and birthing care based on this. Chorionicity relates to the number of placentae and amnionicity to the number of amniotic sacs that will support the babies in utero. These are different qualities to zygosity.
At the earliest scan (should you choose to have them) the sonographer will be looking for the number of placentae and amniotic sacs that they can see alongside multiple babies. The placenta supplies oxygen, nutrients and hormones to the babies and removes waste, whilst the amniotic sac protects them inside its ‘waters’. Identifying chorionicity and amnionicity will help parents and healthcare providers to know what to take into account as pregnancy progresses and is likely to influence decisions in pregnancy and labour.
The chorion is defined by the Oxford English Living Dictionary (11) as ‘the outermost membrane surrounding an embryo of a reptile, bird or mammal. In mammals it contributes to the formation of the placenta’. The chorion develops a system of blood vessels and in association with the lining of the uterus forms the placenta. The placenta is the primary organ supporting nutrition, respiration and excretion for the baby / babies it is attached to (12).
The amnion is defined by the Oxford English Living Dictionary (11) as ‘the innermost membrane that encloses the embryo of a mammal, bird or reptile’. It fills with amniotic fluid to provide a protective environment for the developing fetus. This fluid is ‘the waters’ that surround the baby until they break at the onset of, during, or shortly after, birth.
NICE guidelines for multiples emphasise the importance of determining chorionicity at the time of identifying the twin pregnancy by ultrasound and that if chorionicity is not detectable to seek a second opinion from a senior ultrasonographer as soon as possible (13). Ideally chorionicity will be determined by 13 or 14 weeks gestation (14),(15). So our healthcare system places great store in knowing the type of twins being carried at an early stage.
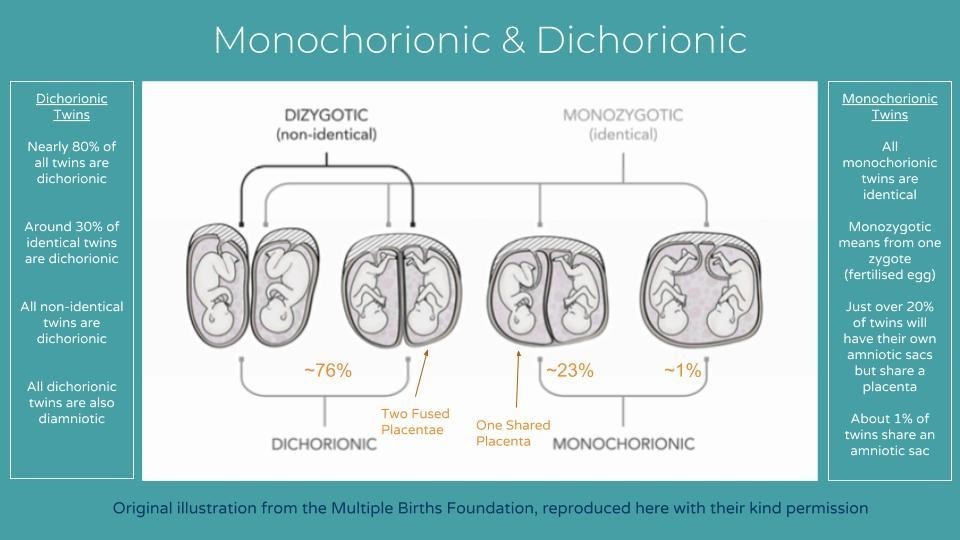
Knowing the number of chorions and amnions in a multiple pregnancy will offer insight into how the babies will be supported by their placenta and protected by their amniotic sac throughout the pregnancy. The terms used to describe types of twins by chorionicity and amnionicity are shown in Figure 2.

The relationship between chorionicity, amnionicity and zygosity is shown in Figure 3. It shows that monozygotic (identical) multiples can present with any chorionicity and amnionicity, whereas dizygotic (fraternal) twins can only be dichorionic and diamniotic. Two placentae fused together can make chorionicity hard to determine; ultrasonically it looks similar to a monochorionic diamniotic structure. If there is any doubt, healthcare providers are advised to offer care as if the pregnancy were monochorionic(13).
Triplets and higher numbers of multiples may show a variety of chorionicity and amnionicity. For example triplets may be trichorionic (each baby having its own placenta), dichorionic (two babies sharing a placenta and one baby having its own, so two placentae in total) or monochorionic (all babies sharing one placenta)(17). Triplets may also be triamniotic, diamniotic or monoamniotic depending on whether there are 1, 2 or 3 amniotic sacs present alongside the babies and their placentae.
The NICE guidelines’ draft care pathway for twin pregnancy outlines the antenatal care you should expect to be offered from your healthcare provider for uncomplicated twin pregnancies and how this differs for monochorionic and dichorionic twin pregnancies. The schedule of care, staff involved (with your consent) and type of care is described in brief.
Chorionicity and Amnionicity Related Conditions
With monochorionic and monoamniotic presentations there are specific conditions that can occur, or are more likely to occur, and so healthcare providers will ask to watch these multiples more closely. Guidelines from the Royal College of Obstetricians and Gynaecologists for professional ‘management of monochorionic twin pregnancies’ are publicly available online. These guidelines state that ‘Clinicians and women should be aware that monochorionic twin pregnancies have higher fetal loss rates than dichorionic twin pregnancies, mainly due to second trimester loss and, overall, may have a higher risk of associated neurodevelopmental morbidity. This should form part of the parental counselling.’ This suggests that women, couples and families pregnantwith monochorionic multiples might need, and should expect, a good deal of information and support from their healthcare provider.
These extra considerations to take on board come about because the placenta is shared. One function of the placenta is to provide a flow of blood to and from the baby. When there is more than one baby the blood flow can become unequal. Imbalances in blood flow can lead to specific medical conditions including: twin-twin transfusion syndrome (TTTS), selective growth restriction (SGR), twin anaemia-polycythaemia sequence (TAPS) and twin reversed arterial perfusion sequence (TRAPS) (15). Conditions relating to shared blood flow are almost universally a consideration for monochorionic pregnancies, however when two placentae fuse there is a slight possibility that blood vessels between the placentae interconnect. This makes it possible for TTTS to occur in these instances but it is very rare (18)
TTTS stands for twin-twin (or twin-to-twin) transfusion syndrome. In higher order multiples the same condition may be referred to as feto-fetal transfusion syndrome (FFTS). This condition affects 10 - 15% of monochorionic twins and usually manifests itself in early pregnancy, typically before 24 weeks. TTTS happens when the blood flow is imbalanced between the multiples sharing a placenta and the ‘recipient’ twin receives a larger share of blood from the placenta, whilst the ‘donor’ twin receives a smaller share. The extra blood being passed to the ‘recipient’ twin can put a strain on this baby’s heart and cause the heart to enlarge. The ‘recipient’ twin will also pass more urine which increases the volume of fluid in its amniotic sac (polyhydramnios). Conversely the ‘donor’ twin may have low blood pressure and become anaemic and dehydrated; its surrounding fluids will decrease (oligohydramnios). The difference in growth between twins with TTTS can become markedly discordant as shown in Figure 4.

Figure 4: An illustration to show the disparity between the growth of twins and the space taken up by their amniotic sacs in TTTS. Reproduced with the kind permission of the Multiple Births Foundation
At the onset of TTTS, sometimes the mother will notice symptoms such as: increased thirst, premature contractions, a notable tightening and swelling of the abdomen, breathlessness and palpitations. There may not be any symptoms, though, and routine and regular ultrasound scans might be the only way the condition is noticed.
Early recognition of TTTS is preferable, so extra ultrasound scans are offered in monochorionic pregnancies. These scans are usually scheduled every two weeks from 16 weeks until 24 weeks. TTTS can be detected by ultrasound. Doppler scans are used to observe blood flow, and ultrasound images can detect any differences in: the amount of amniotic fluid around each baby, the overall size of each baby and its bladder size. If TTTS is detected, the function of the heart will also be recorded in the ‘recipient’ twin.
One half to two-thirds of the sets of babies with TTTS remain stable or improve but will warrant the offer of close monitoring until delivery. The remaining third or so of cases develop into severe TTTS. Currently the best treatment for TTTS is Fetoscopic Laser Ablation Therapy, with a 60% - 70% success rate for survival of both twins, and 10 - 15% for one twin to remain alive. TTTS is a condition taken very seriously by healthcare providers as in its severest form 20% - 25% of twin babies don’t survive (14),(19).
TAPS is a form of twin-twin transfusion in which the monochorionic twins develop markedly different levels of haemoglobin. The ‘donor’ twin can become anaemic, whilst the ‘recipient’ twin displays abnormally high levels of red blood cells which act to thicken blood and slow down its flow. TAPS is harder to identify than TTTS as the levels of amniotic fluid stay balanced, but it can be diagnosed antenatally by Doppler scans and affects between 1% and 6% of monochorionic twins when it occurs spontaneously. TAPS can also occur as a result of fetoscopic laser surgery. Laser surgery is offered to address TTTS, in 16% of laser treated TTTS cases post-laser TAPS occurs. Antenatally, TAPS may be actively managed by laser surgery, intrauterine blood transfusion or if appropriate, early birth through induction or caesarean (20),(21),(22),(23). After birth, a newborn TAPS anaemic twin may require a blood transfusion, whereas the ‘recipient’ with higher Hb levels may be offered a partial exchange transfusion(PET) to redress the imbalance. The PET process is described by MedlinePlus(24) as when ‘a specific amount of the child's blood is removed and replaced with a normal saline solution, plasma (the clear liquid part of blood), or albumin (a solution of blood proteins). This decreases the total number of red blood cells in the body and makes it easier for blood to flow through the body.’
TRAPS is a condition where one twin has a non-functioning heart (called the “acardiac twin”) and the heart of the other twin acts as a pump for both babies, causing a reversed blood flow in the acardiac twin. It is extremely rare and occurs in about 1% of monochorionic twins (25). TRAPS can be detected by ultrasound in the first trimester as the acardiac twin is physically very different to a normal healthy baby. The acardiac twin has no chance of survival as it has no functioning heart of its own and is an abnormal fetus in many physical respects. The ‘pump twin’ however is usually structurally normal, but their heart comes under strain supporting a blood circulation to an extra body. The larger the acardiac twin the greater the strain on the ‘pump’ twin’s heart. Reports of the overall survival rate of the ‘pump’ twin vary widely; 30% - 50% (26), 80% (27) and 90% (28). Expectant management is one treatment option (27), monitoring the normal twin’s heart performance, with the possibility of an elective early birth if the heart becomes significantly compromised. Laser treatment on the unborn baby may also improve survival rates slightly (to 82%), with birth being, on average, at around 37 weeks if laser treatment is received between 13 and 16 weeks (29). Radio Frequency Ablation (described by ‘The Fetal Treatment Center’) which stops the flow of blood into the acardiac twin shows survival rates of up to 90% with birth being, on average, around 35 weeks.
sGR or sIUGR is also a condition that affects multiples sharing a placenta. These acronyms stand for ‘selective growth restriction’ or ‘selective intrauterine growth restriction’. In around 40% of monochorionic pregnancies the placenta is shared disproportionally, which can result in one twin growing slowly whilst the other twin grows at a normal rate. sGR is detected by ultrasound and occurs in 10% - 15% of monochorionic pregnancies. It is defined when there is a weight difference of 25% or more between the twins. There is no way to share the placenta more evenly so currently there is no treatment for sGR. Early delivery of affected multiples is the preferred approach by healthcare providers, with best outcomes for babies born beyond 32 weeks(14),(19).
In monoamniotic pregnancies, when babies are sharing one placenta and one amniotic sac (1% of all twin pregnancies), there is a likelihood that the umbilical cords become entangled, limiting or cutting off essential supplies to one or both twins (15). Women with pregnancies involving a shared amnion should be offered individualised care from healthcare providers with expertise in this area (13).
Multiple pregnancies can be physically demanding on mother and babies, and for the immediate and extended families waiting to welcome the babies a great variety of feelings from many different parts of the emotional spectrum are likely to be experienced along the way. Although for some multiple pregnancies, choices may seem more limited because of their complexities, all decisions are still yours to make. Guidelines suggest at least 2 appointments with a specialist obstetrician for all women carrying twins, plus there are specialist twin midwives within the NHS and independently. These are valuable chances to receive medical information, gain professional support and ask for expert advice about your individual case (13). Of course, who you choose to invite to support your pregnancy is up to you, and knowing more about your type of multiples can help you to decide what type of care is right for you. Being pregnant with two or more babies may draw a certain amount of medical attention, but amidst the medical terminology, machinery and specialist professionals on offer you may need to remind yourself and others that it is your body and your pregnancy, and that ultimately you make the decisions for you and your babies.
References
The AIMS Journal spearheads discussions about change and development in the maternity services..
AIMS Journal articles on the website go back to 1960, offering an important historical record of maternity issues over the past 60 years. Please check the date of the article because the situation that it discusses may have changed since it was published. We are also very aware that the language used in many articles may not be the language that AIMS would use today.
To contact the editors, please email: journal@aims.org.uk
We make the AIMS Journal freely available so that as many people as possible can benefit from the articles. If you found this article interesting please consider supporting us by becoming an AIMS member or making a donation. We are a small charity that accepts no commercial sponsorship, in order to preserve our reputation for providing impartial, evidence-based information.
AIMS supports all maternity service users to navigate the system as it exists, and campaigns for a system which truly meets the needs of all.