AIMS Journal, 2024, Vol 36, No 4

By Bine Browne
The Association of Radical Midwives (ARM) was formed almost fifty years ago in response to the increasing medicalisation of childbirth, expressed in the induction of labour and the active management of labour. Artificial Rupture of Membranes (also ARM) is a key process of labour induction and the word radical was used in the sense of Radix (Lat. “root”) to express the desire of midwives to return to the fundamentals of care “with woman”. Plus ça change and all that. ARM’s central aim has not changed. We remain committed to the midwife woman relationship being the cornerstone of high-quality maternity care. We believe that inappropriate interventions are damaging to mother and baby. The recommendations of ARM’s ‘New Vision’ of Midwifery Care (2012) were expressed by the ‘Better Births’ document published by the government in 2016.
Over the years ARM has regularly highlighted the failings of the NHS maternity service; the over medicalisation leading to inappropriate interventions, the ineffective ways of working, the focus on organisational needs rather than the woman’s needs, the historic underfunding, the bullying culture affecting both service users and staff. It seemed ironic then, that as various reports[1] into individual maternity services in England were published it was the ‘normal birth ideology’ [2] that the media focused on and demonised. The tragic stories of women’s ill treatment by midwives have been hard to read but not altogether unsurprising (though not excusable) given the fear that plagues the staff (both midwifery and obstetric) of most English labour wards. They are afraid of being under investigation, of being reported to the Nursing & Midwifery Council (NMC) and of losing their PIN (registration number).[3] They practise defensively; their main objective is to survive their shift without incident.
Beyond maternity care, we know that all public services are in crisis,[4] that there is an ever increasing gap between rich and poor and that many people are more unhealthy earlier in life because of their poor housing and low incomes and the stress this causes.[5] The impact of stress on maternal and fetal wellbeing is only just beginning to be properly understood.[6]
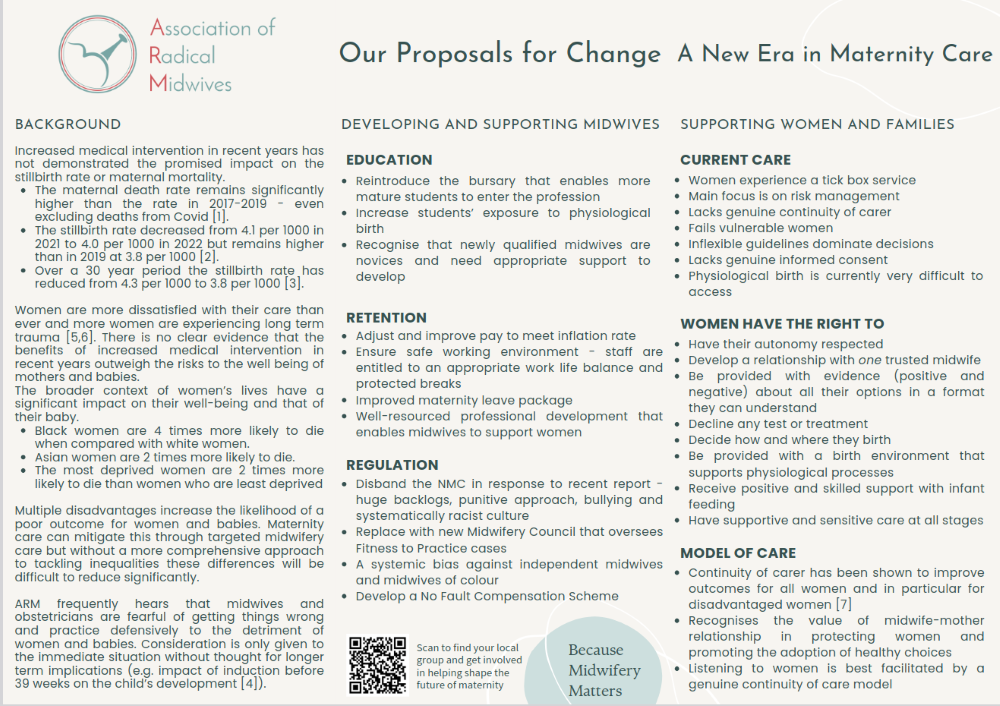
Against this backdrop, and recognising the likelihood of change in government, ARM worked on a pamphlet in June and July that finally was given the hopeful title:
The pamphlet format was chosen as it was thought to be a simple, user-friendly approach to introduce key information, the plan being to send it both electronically and in hard copy to all members of parliament and key stakeholders. We wanted to show that increasing medicalisation isn’t the panacea the media portrays; that improving outcomes for women and babies requires a more nuanced and multi-layer approach that recognises the importance of relational care; that those who care must also feel cared for; that physiology matters; that pregnancy and birth cannot be seen in isolation but rather within the wider societal context.
The five-member group working on the pamphlet represented NHS midwives from various perspectives: a final year midwifery student, a Professional Midwifery Advocate, a midwife working with women to overcome trauma, a caseload midwife, and independent midwifery represented by the fifth member. We also asked those attending our summer meeting to name the two most urgent issues that should be addressed. Drafts were circulated amongst the ARM steering group for further input. In addition, the AIMS Campaign Team kindly reviewed an initial draft providing helpful recommendations which informed the final iteration.
We struggled with the limitations of the format; trying to avoid overloading it with type but not wanting to miss out key information. ARM believes there is an existential crisis in NHS midwifery and the decision to focus on it exclusively was deliberate. The reality of 21st century midwifery care is disturbing and depressing. It is being strangled by a system that values number counting and clock watching.[7] That said, there are still pockets of excellent practice but these are always under pressure to justify their existence and often stretched to the limit when there are staffing issues.[8] There are also midwives who work tirelessly supporting women to birth well against the odds.
We needed to address the core issues: midwifery care is fragmented, there are few opportunities to develop the midwife woman relationship. Midwives are losing their skills in facilitating physiological birth while some midwives have never been exposed to them.[9] We are approaching a point where almost all NHS midwives will only see birth through a medical/obstetric lens.
The pamphlet opens with an overview of the current situation in maternity care. It deliberately begins with the most recent figures available, showing that increased medical intervention in recent years has not demonstrated the promised impact on the stillbirth or maternal mortality rates. This is significant given the level of increase in both the caesarean and induction rates. The caesarean rate in 2023/24 is likely to be above 40% in England (digital.nhs.uk) and while the induction rate is more difficult to obtain accurately, the official rate was 34% in 2022/23,[10] while our members report rates consistently in excess of 40%. This represents an approximate increase of 14% in the former and a very conservative increase of at least 10% in the latter over the last 10 years.
This shift in the way birth happens has consequences for women and their families. It has consequences too for birth workers. There is little spontaneity. Birth is scheduled, women are processed and the maternity unit runs to an assembly line format. The antenatal and postnatal wards become like holding bays; women waiting to be transferred to the labour ward or go home.
The pamphlet speaks about the impact of increasing levels of induction on midwifery workload and the knock-on impact on workload and retention. Most midwives want to provide sensitive, individualised care, but the systems in place don’t support this. Women are having unnecessary interventions often carried out by midwives who do not believe they should be done. Over time, this is demoralising. Midwives either leave or simply switch off.[11] This in turn leads to insensitive and impersonal care that contributes to women’s poor experience and in some cases trauma.
The education of midwives is key to developing a high-quality maternity service. ARM believes it is important that the bursary system is reintroduced to allow for a more diverse workforce and, in particular, mature students and those who have already had children to become midwives. This cohort of students were a regular feature of midwifery courses but since the bursary was abolished, their numbers have fallen dramatically. The bursary is a non-income assessed personal allowance that covers the entire degree programme and allows those with dependents to avoid getting into debt. This system is currently in place in Scotland. All professional groups benefit from greater diversity; midwifery is no exception.
Student midwives’ exposure to physiological birth is very limited, many students never see a spontaneous unmedicated birth.[12] This lack of exposure has been seriously impacted by the increasing rate of inductions. More and more women are falling into a category where induction is recommended but without robust evidence to support it.[13] These categorisations say women are too fat, too thin, too old; their babies are too big or too small. As a result the numbers of women birthing in birth centres has also fallen and the opportunities to attend such births are becoming increasingly rare.[14] Developing experiences via simulation might be way forward. However, the experience of physiological birth in the moment cannot be replaced for its impact on students’ understanding of birth and their development as midwives.
Midwives need to have good pay and working conditions. The new government’s timely pay increase for nurses and midwives has appeased midwives’ concerns about pay for now.[15] However, on-call payments that particularly affect midwives providing caseload care or a home birth service need to be revised upwards to recognise the imposition on one’s personal life and, for example, make it possible for midwives who require paid child care cover to work in this way.
The working conditions of midwives are variable. They regularly report they can’t take their allotted breaks due to staffing levels or high levels of activity. This is obviously not good practice and midwives who are dehydrated and hungry probably can’t be expected to perform to the best of their abilities. Positioning maternity services within secondary health care prevents midwives’ time being used effectively. It also means that women’s time is not considered. If women are concerned during pregnancy, they are expected to ring a helpline and speak with a midwife who doesn’t know them or their circumstances. They may be asked to come to the hospital to be checked. Often, they have to wait hours in a Maternity Triage department. If they were cared for within a caseload model, it is possible their query could be dealt with over the phone by someone who knows their situation or, if needed, be seen closer to home.[16]
Midwives have at least five training days a year to help ensure they remain current in practice developments and skilled in dealing with emergencies. Little or no time is spent in developing midwives’ communication skills, in particular how to support women with decisions around birth. Many midwives are afraid of telling women that they can choose not to be induced, that they can take time to decide what they feel is best for them. They fear push back from management or their clinical colleagues, or they lack confidence in initiating such a discussion. Sometimes, sadly, they don't have the time or motivation. We know from women that it is often the way in which they are treated and spoken to that causes the greatest pain and upset.[17] Midwives need to have time away from the clinical sphere to hear women’s stories and what women need. Some may need additional support to learn new ways of communicating and caring.
There is an ‘obsession’ amongst NHS Trust Risk teams about interpretation of the fetal heart trace using cardiotocography (CTG) monitoring in labour. The CTG monitor has repeatedly been shown to be a very poor screening tool for fetal wellbeing and yet the number of training hours spent on it are considerable.[18] This time could be better spent on helping midwives to understand what women need from them on their childbearing journey.
ARM believes that the Nursing & Midwifery Council (NMC) should be replaced by a new regulatory body led by professional and lay experts, and that the current Fitness to Practise model needs to be completely transformed to one that is compassionate, learning, retentive, and upholds women's choices and autonomy. The NMC is a dysfunctional organisation with a punitive approach to registrants, backlogs of more than five years, and according to Nazim Afzal’s Independent Cultural Review,[19] has a culture of systemic bullying and racism. There is a deep-rooted bias against midwives of colour and independent midwives. Many cases have been dragging on for years only for the registrant to be found to have no case to answer when the hearing finally takes place. Midwives are emotionally and financially drained and often decide to come off the register, despite not having done anything wrong other than facilitate women's choice. In some tragic cases they have been known to take their own lives or suffer long-term health problems. It is estimated that at least 27 midwives and nurses have committed suicide following referral to the NMC since 2016.[20]
ARM wants every woman to have the option of their own named midwife with whom they can develop a trusted relationship to see them through their childbearing journey. The midwife would be part of a small team locally based and with each midwife having a defined caseload of women. We know the continuity of carer model works for women and, in particular, disadvantaged groups. It has been recommended by numerous reports into maternity care and there is a large body of evidence to support its positive impact on maternal and newborn outcomes.[21] It works for midwives too, if it is correctly resourced and supported. Implementing this model of care requires commitment, resources and a vision for the maternity service that values the woman’s voice above all others.
ARM believes that midwives need support to support women. We believe that this pamphlet can be used as a guide to best achieve this aim. We encourage all to send and share it with colleagues and MPs to raise awareness and encourage change. AIMS welcomed Wes Streeting in August and presented a powerful argument for the development of continuity of carer model as the standard for all women. We hope we can work collaboratively with AIMS to make this a reality.
Author Bio: Bine (Abina) Browne has been a midwife since 1984. She has worked in education, management and most recently as a caseload midwife for vulnerable women.
She retired in September.
MBRRACE-UK. (2023). Saving lives, improving mothers’ care: Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2019-21. www.npeu.ox.ac.uk/assets/downloads/mbrrace-uk/reports/maternal-report-2023/MBRRACE-UK_Maternal_Compiled_Report_2023.pdf
Office for National Statistics. (2023). Births in England and Wales: 2022. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthsummarytablesenglandandwales/2022
Office for National Statistics. (2021). Birth characteristics in England and Wales: 2020. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthcharacteristicsinenglandandwales/2020
Burger, R. J., Mol, B. W., Ganzevoort, W., Gordijn, S. J., Pajkrt, E., Van Der Post, J. A. M., De Groot, C. J. M., & Ravelli, A. C. J. (2023). Offspring school performance at age 12 after induction of labor vs non-intervention at term: A linked cohort study. Acta Obstetricia et Gynecologica Scandinavica, 102(4), 486–495. https://doi.org/10.1111/aogs.14520
Care Quality Commission. (2024). Maternity survey 2023. www.cqc.org.uk/publications/surveys/maternity-survey#:~:text=At%20a%20national%20level%20the,from%20between%202018%20and%20202
Thomas, K. (2024). A report by The All-Party Parliamentary Group on Birth Trauma. Secretariat of the APPG on Birth Trauma and CEO of the Birth Trauma Association. Accessed: www.theo-clarke.org.uk/sites/www.theo-clarke.org.uk/files/2024-05/Birth%20Trauma%20Inquiry%20Report%20for%20Publication_May13_2024.pdf
[1] Kirkup, B. (2015). The Report of the Morecambe Bay Investigation. Department of Health.
URL: www.gov.uk/government/publications/morecambe-bay-investigation-report
[2] Wilson, C. (2023, October 30). How the battle over ‘normal’ births is still damaging NHS maternity care. iNews. https://inews.co.uk/news/how-the-battle-over-normal-births-is-still-damaging-nhs-maternity-care-3285447
[3] Alexander, C. R., & Bogossian, F. (2018). Midwives and clinical investigation: A review of the literature. Women and Birth, 31(6), 442-452. https://doi.org/10.1016/j.wombi.2018.02.003
[4] Dunn, P., Ewbank, L., & Alderwick, H. (2023, November 3). Nine major challenges facing health and care in England. The Health Foundation. www.health.org.uk/publications/long-reads/nine-major-challenges-facing-health-and-care-in-england
[5] Kulakiewicz, A. (2022, October 17). Housing and health: A reading list (Research Briefing CBP-9414). House of Commons Library. https://commonslibrary.parliament.uk/research-briefings/cbp-9414
[6] Coussons-Read, M. E. (2013). Effects of prenatal stress on pregnancy and human development: Mechanisms and pathways. Obstetric Medicine, 6(2), 52–57. https://doi.org/10.1177/1753495X12473751
[7] Derry, R. (2008).The Tyranny of Time: Tensions between Relational and Clock Time in Community-Based Midwifery. November 2008. Social Theory & Health 6(4):342-363. DOI:10.1057/sth.2008.13
[8] Reed, B., & Edwards, N. (2023). Closure: How the flagship Albany Midwifery Practice, at the heart of its South London community, was demonised and dismantled (1st ed.). Pinter & Martin.
[9] Darling, F., McCourt, C., & Cartwright, M. (2021). Facilitators and barriers to the implementation of a physiological approach during labour and birth: A systematic review and thematic synthesis. Midwifery, 92, Article 102861. https://doi.org/10.1016/j.midw.2020.102861
[10] NHS Digital. (2023). NHS maternity statistics, England, 2022-23: Deliveries - time series. NHS Digital. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-maternity-statistics/2022-23/deliveries---time-series
[11] Barker, K. (2016, December 2). Reasons why midwives leave. BMJ, 24(12)
[12] Davison, C., Ritchie, E., & Watts, N. (2023). Midwifery students’ confidence to support physiological birth: An international study. Women and Birth, 36(Supplement 1), S1. https://doi.org/10.1016/j.wombi.2023.0g7.003
[13] Middleton, P., Shepherd, E., Morris, J., Crowther, C. A., & Gomersall, J. C. (2020). Induction of labour at or beyond 37 weeks' gestation. Cochrane Database of Systematic Reviews, 2020(7), CD004945. https://doi.org/10.1002/14651858.CD004945.pub5
[14] Coxon, K., Chisholm, A., Malouf, R., Rowe, R., & Hollowell, J. (2017). What influences birthplace preferences, choices and decision-making amongst healthy women with straightforward pregnancies in the UK? A qualitative evidence synthesis using a ‘best fit’ framework approach. BMC Pregnancy and Childbirth, 17, Article 103. https://doi.org/10.1186/s12884-017-1279-7
[15] Church, E. (2024, July 29). Nurse pay to rise by 5.5% for 2024-25, government confirms. Nursing Times. www.nursingtimes.net/policies-and-guidance/nurse-pay-to-rise-by-5-5-for-2024-25-government-confirms-29-07-2024
[16] Forster, D. A., McLachlan, H. L., Davey, M.-A., Biro, M. A., Farrell, T., Gold, L., Flood, M., Shafiei, T., & Waldenström, U. (2016). Continuity of care by a primary midwife (caseload midwifery) increases women’s satisfaction with antenatal, intrapartum and postpartum care: Results from the COSMOS randomised controlled trial. BMC Pregnancy and Childbirth, 16, Article 28. https://doi.org/10.1186/s12884-016-0831-0
[17] Thomas, K. (2024). A report by The All-Party Parliamentary Group on Birth Trauma. Secretariat of the APPG on Birth Trauma and CEO of the Birth Trauma Association. Accessed: www.theo-clarke.org.uk/sites/www.theo-clarke.org.uk/files/2024-05/Birth%20Trauma%20Inquiry%20Report%20for%20Publication_May13_2024.pdf
[18] Small, K. A., Sidebotham, M., Fenwick, J., & Gamble, J. (2020). Intrapartum cardiotocograph monitoring and perinatal outcomes for women at risk: Literature review. Women and Birth, 33(5), 411–418. https://doi.org/10.1016/j.wombi.2019.10.002
[19] Rise Associates. (2024). The Nursing and Midwifery Council independent culture review: July 2024. Nursing and Midwifery Council. www.nmc.org.uk/globalassets/sitedocuments/independent-reviews/2024/nmc-independent-culture-review-july-2024.pdf
[20] Devereux, E. (2024, July 25). Fitness to practise: 16 die by suicide while under investigation. Nursing Times. www.nursingtimes.net/professional-regulation/fitness-to-practise-16-die-by-suicide-while-under-investigation-25-07-2024
[21] Sandall, J., Fernandez Turienzo, C., Devane, D., Soltani, H., Gillespie, P., Gates, S., Jones, L. V., Shennan, A. H., & Rayment-Jones, H. (2024). Are midwife continuity of care models versus other models of care for childbearing women better for women and their babies? Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD004667.pub5
The AIMS Journal spearheads discussions about change and development in the maternity services..
AIMS Journal articles on the website go back to 1960, offering an important historical record of maternity issues over the past 60 years. Please check the date of the article because the situation that it discusses may have changed since it was published. We are also very aware that the language used in many articles may not be the language that AIMS would use today.
To contact the editors, please email: journal@aims.org.uk
We make the AIMS Journal freely available so that as many people as possible can benefit from the articles. If you found this article interesting please consider supporting us by becoming an AIMS member or making a donation. We are a small charity that accepts no commercial sponsorship, in order to preserve our reputation for providing impartial, evidence-based information.
AIMS supports all maternity service users to navigate the system as it exists, and campaigns for a system which truly meets the needs of all.