AIMS Journal, 2024, Vol 36, No 4

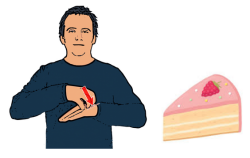
Sign images from british-sign.co.uk
By Alex Smith
Welcome to the December 2024 edition of the AIMS journal. The theme for this quarter considers the experience of care for deaf1 parents and also for parents who discover that their baby is deaf. We have called this issue, ‘The Deafness Loop (with a nod to the hearing loop): a cycle of inequality’. This is because the inequalities that deaf babies born today will face from birth and throughout their education, are directly connected to the inequalities that Deaf parents face throughout their maternity care.
As we know, feeling traumatised after a poor experience of maternity care is a growing problem. 2, 3 Communication issues are often implicated in lasting feelings of trauma, and MNSI (the Maternity and Newborn Safety Investigations group) says that:
“Communication is a key patient safety systems issue in maternity care, as well as being a significant determinant in families’ experiences.”4
If determined, well-prepared, hearing parents find it hard to communicate and to be heard, just imagine how much harder it is for Deaf parents - especially those with British Sign Language (BSL) as a first language.
Meghan Luton who writes in this issue, has conducted research5 showing that compared with hearing parents, Deaf parents are less likely to have incidental knowledge about healthcare systems, about their rights, and about medical terminology. Incidental knowledge is the sort of knowledge acquired from overheard discussions, chatting with friends, or from television and radio. This means that Deaf people are more likely to be attending appointments without even knowing why. They may ‘consent’ to a procedure without knowing its purpose; for example, they may think an examination is a routine check when it is actually the first step of an induction. And Deaf women are less likely to speak up for themselves.
This shocking situation is also explained by recent research that reveals a discrepancy between midwives’ actual knowledge of legal consent (poor) and their self-perceptions of their knowledge (excellent). It concluded that midwives urgently require further training to ensure that their consent practices are compliant with the law.6
For anyone - parent or practitioner - this is a reminder about medical consent.7, 8
Your consent is required for every test, examination, procedure or treatment.
Consent is only validly obtained when all reasonable options are on offer, including the option to say no to any or all of them, in other words, the option to do nothing.
Consent is only validly obtained when the medical practitioner takes reasonable care to ensure that the person understands the actual balance of risks and benefits between each option.
Consent can be withdrawn at any time before or even during a procedure and the practitioner must stop immediately if you have asked them to. Of course, in some situations there may be a ‘no turning back’ point, for example, once a caesarean incision has been made, but even then the surgeon should pause and listen to your concerns.9
If this is new information, give yourself a moment to absorb it. Tea?

The following uninformed or reluctant ‘agreements’ are not consent.
Agreeing to care without knowing its purpose - is not consent.
Agreeing to something without feeling you have an option - is not consent.
‘Coaxed-compliance’ - compliance gained with smiles and gentle words - is not consent
Compliance gained through veiled or partly veiled threats - is not consent. “Yes, you do have a choice, but we don’t want anything to happen to the baby, do we.” Is like saying, “Do as we say, and no-one gets hurt.” It is a hostage situation.
Saying yes to something when the risks have been overinflated - is not consent.
And ‘NO’ conveyed as facial expression or body language still means no.
This needs to be crystal clear to every health practitioner and every service user - including BSL users and BSL interpreters. If every hospital, surgery or clinic waiting room had a screen with consent being explained in BSL, with voice and subtitles and other language options, both Deaf and hearing service users, as well as the staff who would see this every day, would be reminded. This video from the Scottish government, but relevant throughout the UK, explains medical consent and the patient’s rights in BSL.
Meghan’s research[5] also shows that Deaf women are more likely to delay or avoid care (a fact that is also true for Deaf women in the States10 and probably globally11) and that satisfaction with care decreases as the number of appointments increase. This makes good sense. If appointments feel rushed, impersonal, uncaring, confusing and insensitive, and when Deaf parents feel powerless, then lying low seems entirely rational. Deaf women are often routinely treated as ‘high risk’, denied access to physiology-informed care, and experience invasive procedures without any choice in the matter.12 It must feel like walking into the lion’s den. While hearing women have the option of calling for a quick chat to sort out concerns, Deaf women do not. One-to-one midwifery would enable the midwife caring for a Deaf woman (and/or her Deaf partner) to understand this person’s preferred method of making contact so that communications can be straightforward and timely, but less than one quarter of women in the UK benefit from seeing the same midwife at each visit.13
Neither Deaf nor hearing women have any legal obligation to engage with the maternity services more than they wish to. However, the research shows that the minority of Deaf women with health conditions that would benefit from good medical care is somewhat higher than it is for hearing women. This makes it particularly important that everything should be in place to ensure that Deaf women feel welcomed, respected and able to communicate freely and without rush. To this end, a professional, specialist interpreter is essential.
Sign Language Interpreters are highly qualified. They have level 6 in BSL and Interpreter training on top of that, but as of November 2022, there were only 908 registered BSL interpreters and 234 trainees. Research shows that accessing an interpreter in a healthcare setting can be difficult.14 Some NHS trust websites require anything from 3 days to 3 weeks notice for bookings, and when an interpreter is not available, is delayed or does not appear, family members, or staff with very basic BSL, may be used instead. This is not always sufficient or safe. Online BSL interpreting agencies like SignLive and SignVideo can be more instantly available - presumably woefully inadequate in these situations but possibly better than nothing.
A good interpreter makes all the difference, but one thing an interpreter isn’t is a doula. If the doctor or midwife says, “I need to examine you now”, the interpreter signs just that. In some ways the mother is being told twice. The interpreter does not add, “But you can say no.” If the mother looks reluctant, but submits, the interpreter does not intervene to remind the doctor or midwife to go through the consent process properly. This would be against their professional code. The hospital is funding the interpreter and in some ways the interpreter is supporting the status quo.
The British Sign Language (BSL) Act 202215 means that there is now a legal duty to provide the correct communication support for Deaf British Sign Language users in the UK. But, according to Lesley Weatherson whose very interesting 2022 article is republished in this issue, the Act is either being ignored, is not understood or is not known about.16 This disregard for the law also appears to be the case for hearing impaired people who rely on spoken English, as Helen Jones found. She writes in her account:
“It was written in my notes that I was hearing impaired but no one seemed to take any notice of this.”
It might be reasonable to assume that good written information would fill the communication gap, but as I explain in another article in this issue, ‘Why can’t we just give deaf people a leaflet?’, this isn’t always the case. A further page from me covers a miscellaneous selection of ‘Did you know?’ information about deafness and maternity.
Imagining how another person experiences the world is hard. Cake?
We continue the theme of deafness and pregnancy with three contributors writing about their experience of having a baby diagnosed with deafness. In ‘A child is born into the world and their world is in silence’, the mother writes about her struggle to provide language for her child, and about the educational inequalities that Deaf children endure; Karrie, whose child is still very young, talks about her initial shock, and her determination to help her son develop a positive Deaf identity; and a third mother shares her appalling experience of her early encounters with the audiology department, that seem completely devoid of empathy, compassion or useful information, but ends up feeling very positive about the results of the care her son received. To conclude the themed section of the journal we have a delightful bite-sized article from Salli Ward, telling us about the first baby to have their BSL sign name legally recorded on their birth certificate.
Moving on, Catharine Hart reports on the Microbirth summit, and we have our regular Birth Activist Briefing, on this occasion about the Maternal Mental Health Service Progress report. Bine Browne, retired midwife and member of the Association of Radical Midwives (ARM), introduces us to the ARM’s pamphlet, ‘Proposals for Change : A New Era in Maternity Care’. Jo Dagustun tells us about an interesting NHS conference she attended recently, and in a further article Jo explains why AIMS is calling for a full pathway continuity of carer model of care to be a key plank of the new Government’s renewed maternity transformation policy. We also have a second piece from Catharine Hart in which she tells us about the Cochrane review that compares outcomes for women and babies who received midwife continuity of care with other models of care. Last, but never least, the AIMS Campaign’s Team tells us what they have been up to since September.
We are very grateful to all the volunteers who help in the production of our Journal: our authors, peer reviewers, proofreaders, website uploaders and, of course, our readers and supporters. This edition especially benefited from the help of Anne Glover, Jo Dagustun, Jo Williams, Danielle Gilmour, Katherine Revell, Salli Ward and Josey Smith.
We have a two-fold theme for the March 2025 issue of the AIMS journal. The first is on becoming a grandparent , and the second is on generational trauma or resilience. If those potentially related topics stir ideas, insights or stories that you would like to share, please contact me at: alex.smith@aims.org.uk
Author Bio: Alex Smith is a long-time childbirth educator, the editor of the AIMS journal and a proud grandmother of a profoundly deaf grandson.
1 Editor’s note: A capital ‘D’ is used when indicating someone who identifies themselves as culturally Deaf and part of the Deaf community. https://hearmeoutcc.com/capital-d-small-d-deaf
2 Parliamentary Inquiry into Birth Trauma: Call for Evidence - AIMS Submission
www.aims.org.uk/campaigning/item/parliamentary-inquiry-birth-trauma
3 AIMS (2024) Birth Trauma Inquiry Open Letter - May 2024
www.aims.org.uk/campaigning/item/birth-trauma-inquiry-open-letter
4 MNSI (2023) Safety factors surrounding effective communication throughout the pregnancy journey
www.mnsi.org.uk/news/safety-factors-and-effective-communications-in-pregnancy
5 Luton M. (2022) Deaf women’s experiences of maternity and primary care: an integrative review https://repository.mdx.ac.uk/download/d1c3cfaa85d9e2bced85d5397db9fdc616bc617b4deb4f18e0fa272fe36d0a1d/266790/DeafWomensExperiencesOfMaternityAndPrimaryCare.pdf
6 Elf R., Nicholls J., Ni Y., Harris J., Lanceley Anne. (2023) Consent practices in midwifery: A survey of UK midwives. Midwifery, Volume 129, 103893, ISSN 0266-6138
7 AIMS (2020) Making decisions about your care. www.aims.org.uk/information/item/making-decisions
8 Birthrights (2021) Consent: the key facts. https://birthrights.org.uk/factsheets/consenting-to-treatment
9 British Medical Association (2024) Ethics Toolkit Consent and refusal by adults with decision-making capacity. www.bma.org.uk/media/txrnpo3s/consent-refusal-toolkit2024.pdf
10 Lerner, M. (2023). Pregnancy Experiences of Deaf People. National Center
for Disability and Pregnancy Research, Brandeis University, Waltham, MA. https://heller.brandeis.edu/disability-and-pregnancy/pdfs/briefs/pregnancy-experiences-of-Deaf-people.pdf
11 Adigun, O.T.; Akinrinoye, O.; Obilor, H.N. Including the Excluded in Antenatal Care: A Systematic Review of Concerns for D/deaf Pregnant Women. Behav. Sci. 2021, 11, 67. https://doi.org/10.3390/bs11050067
12 Inequalities AND Unreasonable Adjustments: Are D/Deaf women being given a detrimental care pathway in the name of risk assessment? www.all4maternity.com/inequalities-and-unreasonable-adjustments-are-d-Deaf-women-being-given-a-detrimental-care-pathway-in-the-name-of-risk-assessment
13 Dodsworth E. (2023) Inequalities in midwifery continuity of care during pregnancy
www.nuffieldtrust.org.uk/news-item/inequalities-in-midwifery-continuity-of-care-during-pregnancy
14 SignHealth (2014) Sick of It. London: SignHealth. https://signhealth.org.uk/resources/report-sick-of-it
15 The British Sign Language (BSL) report 2022. www.gov.uk/government/publications/the-british-sign-language-bsl-report-2022/the-british-sign-language-bsl-report-2022
16 Weatherson L. (2022) Support for Deaf and Deafblind women in the maternity setting. https://maternityandmidwifery.co.uk/support-for-Deaf-and-Deafblind-women-in-the-maternity-setting
The AIMS Journal spearheads discussions about change and development in the maternity services..
AIMS Journal articles on the website go back to 1960, offering an important historical record of maternity issues over the past 60 years. Please check the date of the article because the situation that it discusses may have changed since it was published. We are also very aware that the language used in many articles may not be the language that AIMS would use today.
To contact the editors, please email: journal@aims.org.uk
We make the AIMS Journal freely available so that as many people as possible can benefit from the articles. If you found this article interesting please consider supporting us by becoming an AIMS member or making a donation. We are a small charity that accepts no commercial sponsorship, in order to preserve our reputation for providing impartial, evidence-based information.
AIMS supports all maternity service users to navigate the system as it exists, and campaigns for a system which truly meets the needs of all.